The following medical billing and coding Guidance, for COVID-19 vaccines, ONLY applies to New York Providers.
As per MVP: ALL COVID-19 vaccines are covered for all PLANS without a member cost-share.
In order to get reimbursement, providers need to follow the proper COVID-19 vaccine billing and coding guidance.
For MVP Medicare Patients:
Providers please bill Medicare Fee-for-Service (FFS) directly for the vaccine and administration of the
vaccine to MVP Members enrolled in Medicare Advantage in 2020 and 2021. If Providers will bill the COVID-19 claims to MVP, they will be denied.
For MVP Commercial and Managed Medicaid Patients:
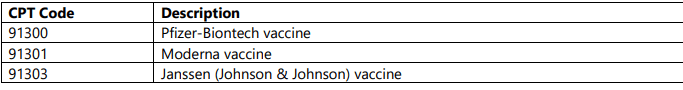
Since COVID-19 vaccines are provided by the government at no charge, Providers should not bill the Vaccine codes (please see below Picture 2). Instead providers should only bill the administration codes (see below Picture 1).

MVP will reimburse both In Network and Out of Network providers.
- Tufts Health One Care: New Plan name and ID cards
- Fidelis MMC: healthy nutrition benefit
- UHC Medicaid: Idaho: diabetic DME coverage change-benefit
- Anthem BCBS: 32BJ fund new TPA and cards
- Are you leaving revenue on the table?

