In this blog post I will provide links to the various states where UHC has a Medicaid plan that added new codes to their prior authorization lists.
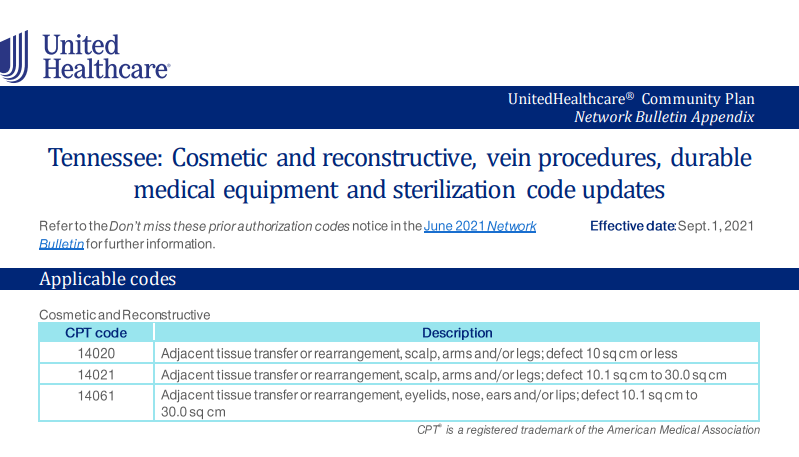
Effective Sept. 1, 2021, we are adding new codes to the prior authorization list for UnitedHealthcare Community Plans (Medicaid, Long-Term Care) in Florida, Mississippi, New Jersey, Pennsylvania and Tennessee.
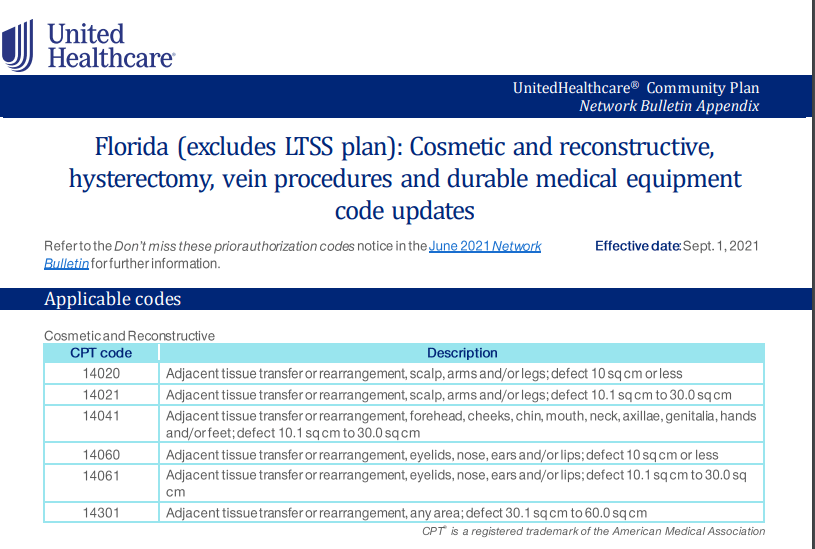
If you would like to see the full list, please click here.
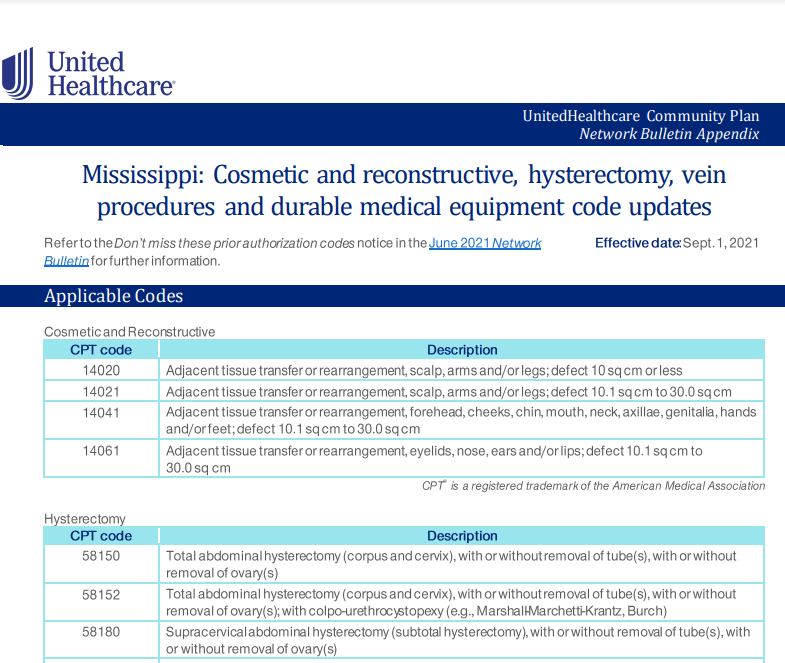
If you would like to see the full list, please click here.
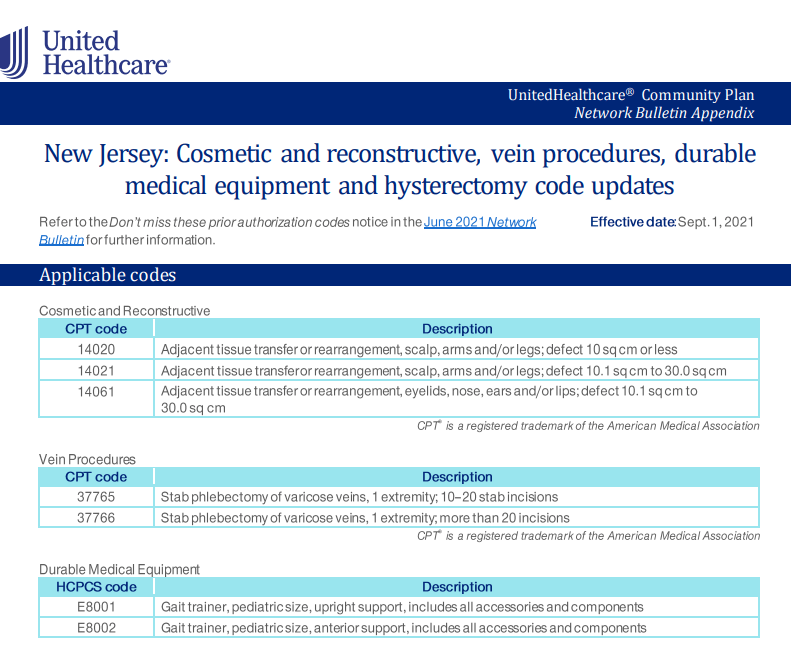
If you would like to see the full list, please click here.
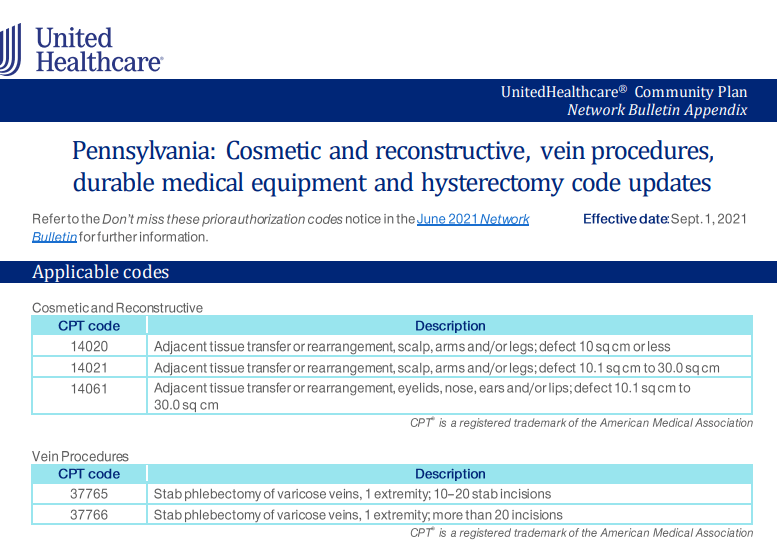
If you would like to see the full list, please click here.
If you would like to see the complete list, please click here.
Find this content helpful? Follow my blog for more medical billing and coding training. Stay current with various insurance plan changes. Would like to learn on demand? Visit my on-demand page for more information.
Recent Blog Posts:
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.


Howdy, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam feedback? If so how do you stop it, any plugin or anything you can suggest? I get so much lately it’s driving me crazy so any help is very much appreciated.