If you are a provider that accepts patients with EmblemHealth and/or Connecticare Insurance this blog post is for you!
This policy applies to Emblemhealth/Connecticare Commercial, Medicare and Medicaid Members.
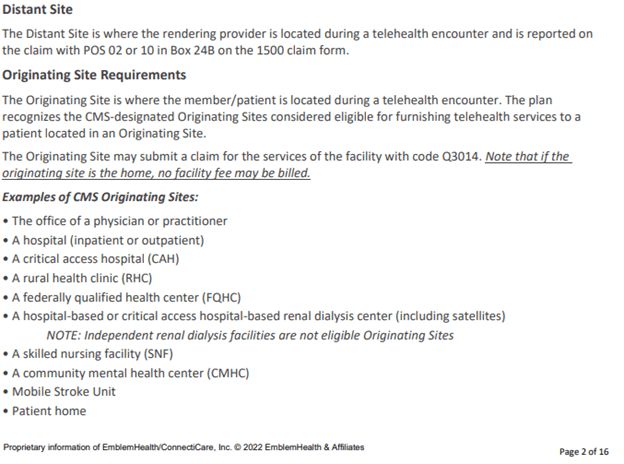
Effective 01/01/2022- EmblemHealth/Connecticare has updated their telehealth policy. The following update was added:

Effective 06/01/2022- changes effect modifiers:

Want to learn more? Please click here to see the whole telehealth policy.
Recent Blog Posts:


i paid out of pocket for pain medications
Hi, Brenda- There are several reasons why you would pay for pain medication out of pocket. The most common one is either high deductible or you have a coinsurance and a high out of pocket limit. You will continue to pay for the pain medications out of your pocket, until you meet your deductible and then your out of pocket, at which time the insurance will start covering you at 100%.