Starting 01/01/2023 Oxford will add and remove certain codes that require prior authorizations (commercial line of business).
According the Oxford this change helps align their processes with evidence-based clinical guidelines.
Some of the new codes that will be added are:
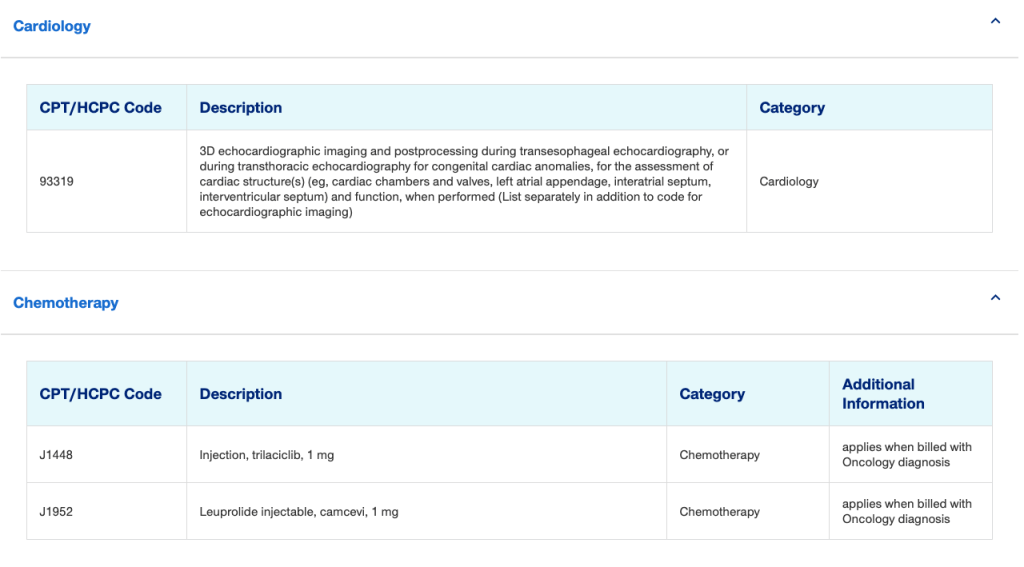
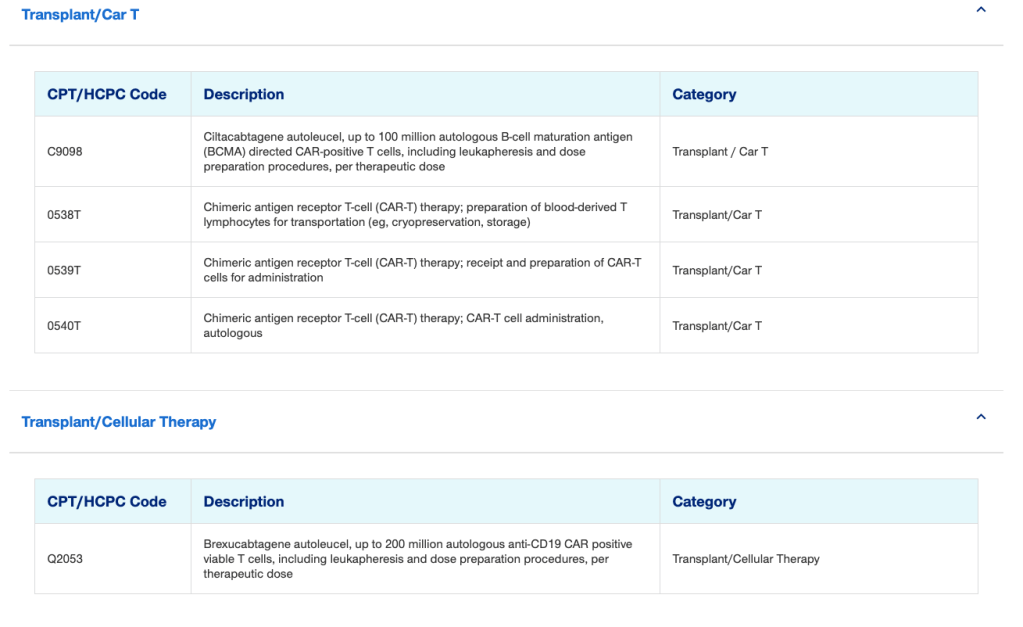
For a full list of new codes that will be added to the list of codes that require prior authorization, please click here.
In addition Oxford is also adding a new provider tool, the UnitedHealthcare Oxford plan Prior Authorization Requirements document, it will become available as of Dec. 1, 2022, on the Advance Notification and Clinical Submission Requirements page.
Providers are encouraged to use this tool where they will be able to find/research codes that require prior authorization as well as request an auth.
Would you like to learn more: please click here, for the Applicable Oxford Commercial policies.
Find this type of content useful? Subscribe and follow my blog/web for everything new medical billing and coding.
Recent Blog Posts:
- Tufts Health One Care: New Plan name and ID cards
- Fidelis MMC: healthy nutrition benefit
- UHC Medicaid: Idaho: diabetic DME coverage change-benefit
- Anthem BCBS: 32BJ fund new TPA and cards
- Are you leaving revenue on the table?
#medicalcoding, #medicalbilling, #priorauthorization, #cardiology, #uhc, #oxford

