Please note that this policy update applies to the members that have commercial plan types.
The affected codes: for any DOS on or after Jan 1st 2026, Aetna will consider the following codes for compression stockings to be a disposable supply and a standard benefit exclusion.
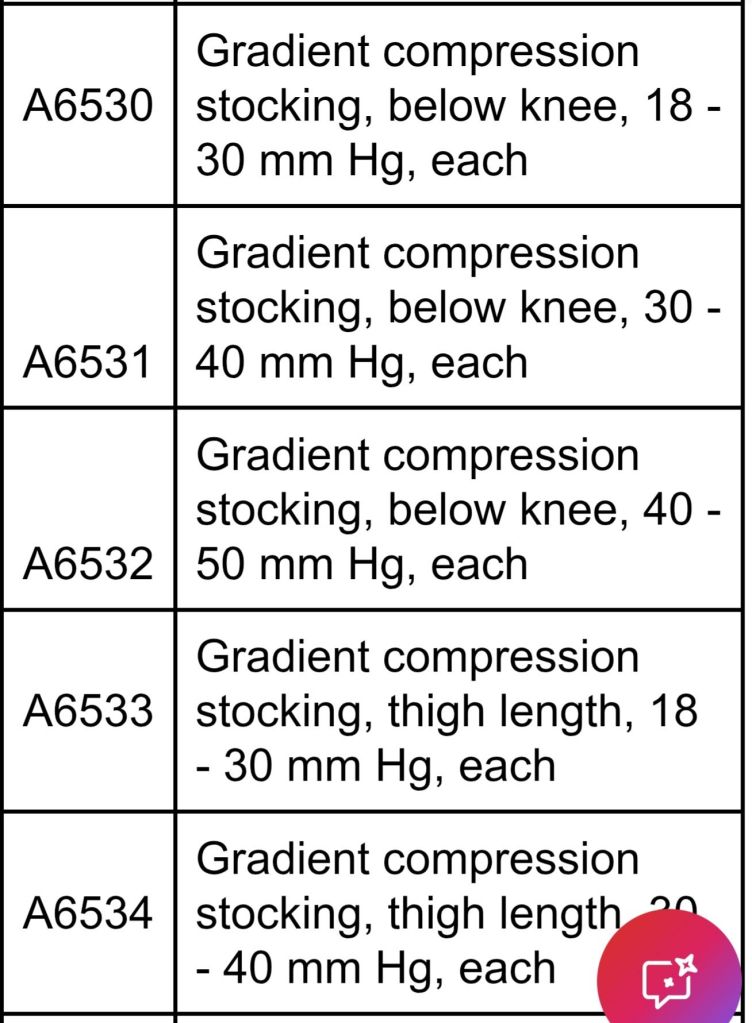
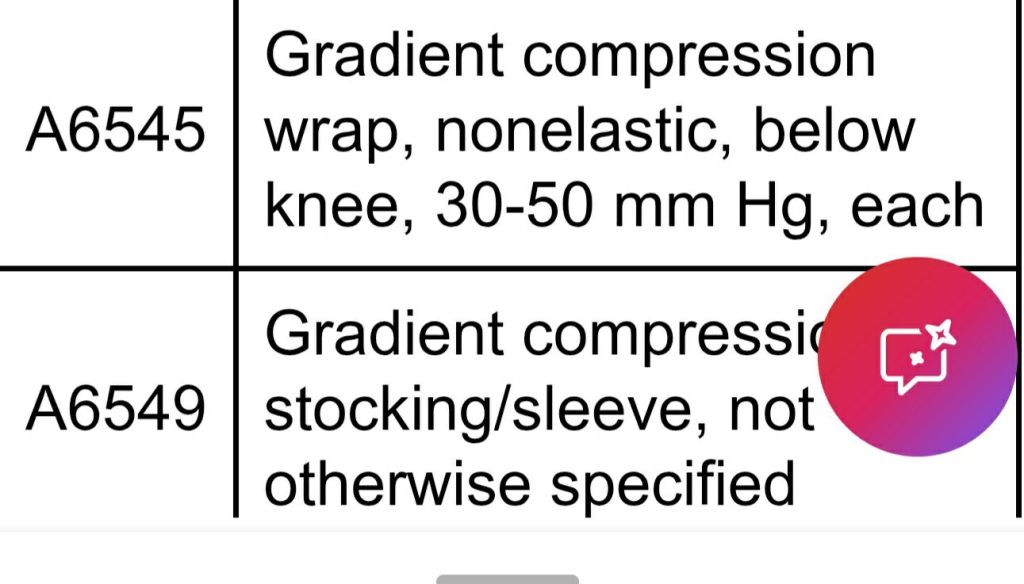
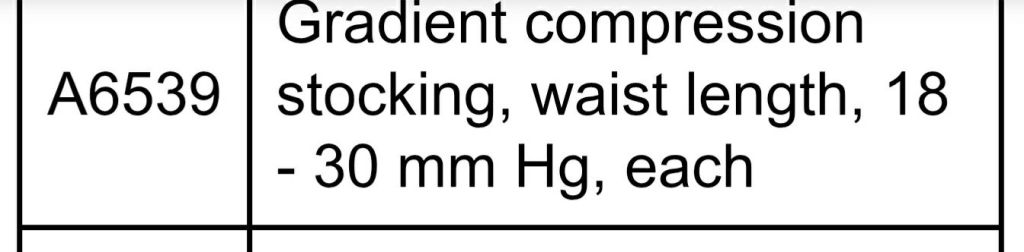
Codes:
For Texas Providers:
These changes apply to fully insured plans written in Texas and only if such changes are in accordance with applicable regulatory requirements. Changes for all other plans will be as outlined in this article.
Find this type of content useful? Follow my blog for more payer updates. #medicalbilling #medicalcoding #reimbursement
- UHC Community Health of Fl- new transportation provider
- Carolina Complete Health: radiology and diagnostic cardiology prior auth update
- NYS Medicaid: existing policy reminder coverage for SD/ED
- Carolina Complete Health: co-pays for pregnant members info
- HEDIS Measure: Lead Screening in Children (LSC)

Leave a comment