This update applies to HealthFirst following plan types: Medicaid, Personal Wellness Plan (HARP), and Medicaid Advantage.
Which services are affected?
Telehealth services done through a NY OMH licensed and or designated outpatient program.
Please refer to OMH modifier and rate code chart here.
To ensure the providers receive proper reimbursement, please make sure you go over payment rate changes and use the proper modifiers:
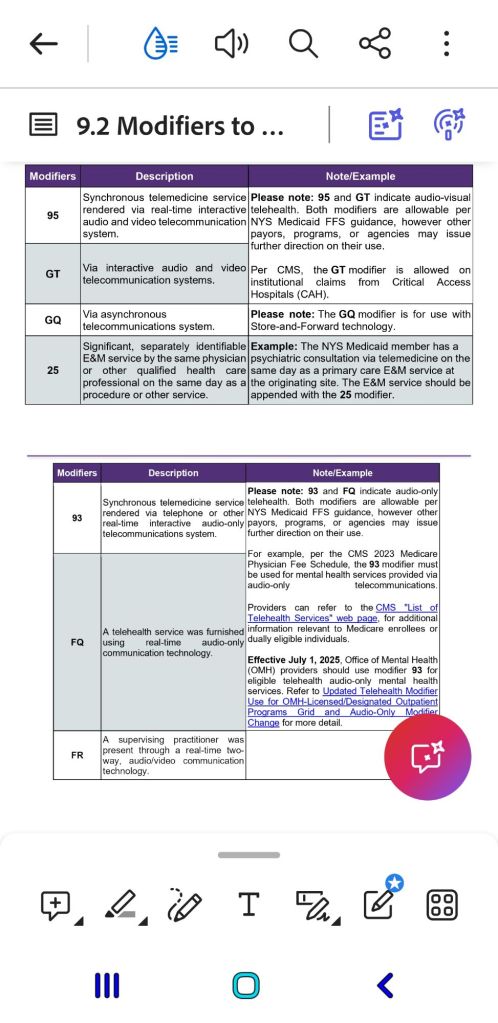
Modifier FQ- used for outpatient telehealth services, audio-only, for dual enrolled members.
Modofier 93- OMH providers – use this modifier for qualifying telehealth and audio-only mental health services, for members that are only enrolled in Medicaid.
The changes apply to the services performed on or after July 1st 2025.
Find this type of content useful? Follow my blog for more useful payer updates, medical billing, coding and reimbursement updates.
- UHC Community Health of Fl- new transportation provider
- Carolina Complete Health: radiology and diagnostic cardiology prior auth update
- NYS Medicaid: existing policy reminder coverage for SD/ED
- Carolina Complete Health: co-pays for pregnant members info
- HEDIS Measure: Lead Screening in Children (LSC)

Leave a comment