The information discussed below applies to straight NYS Medicaid members for the DOS 10/1/25 and effective for any DOS on or 11/1/25 and thereafter for any Managed Medicaid Members.
What is TC? A non-invasive form of brain stimulation using magnetic pulses on specific areas of the brain. This therapy is used to improve the symptoms of major depressive disorder when conventional treatments have failed.
Who can perform these services?
A qualified psychiatrist with specialized training and certification.
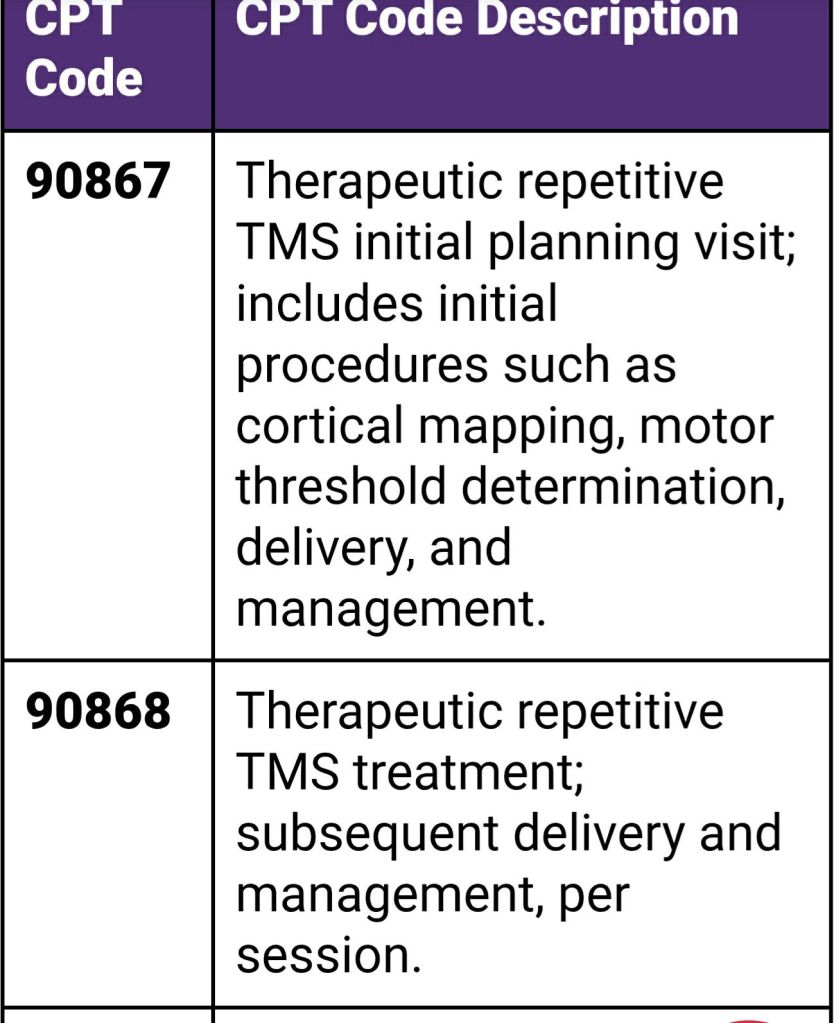
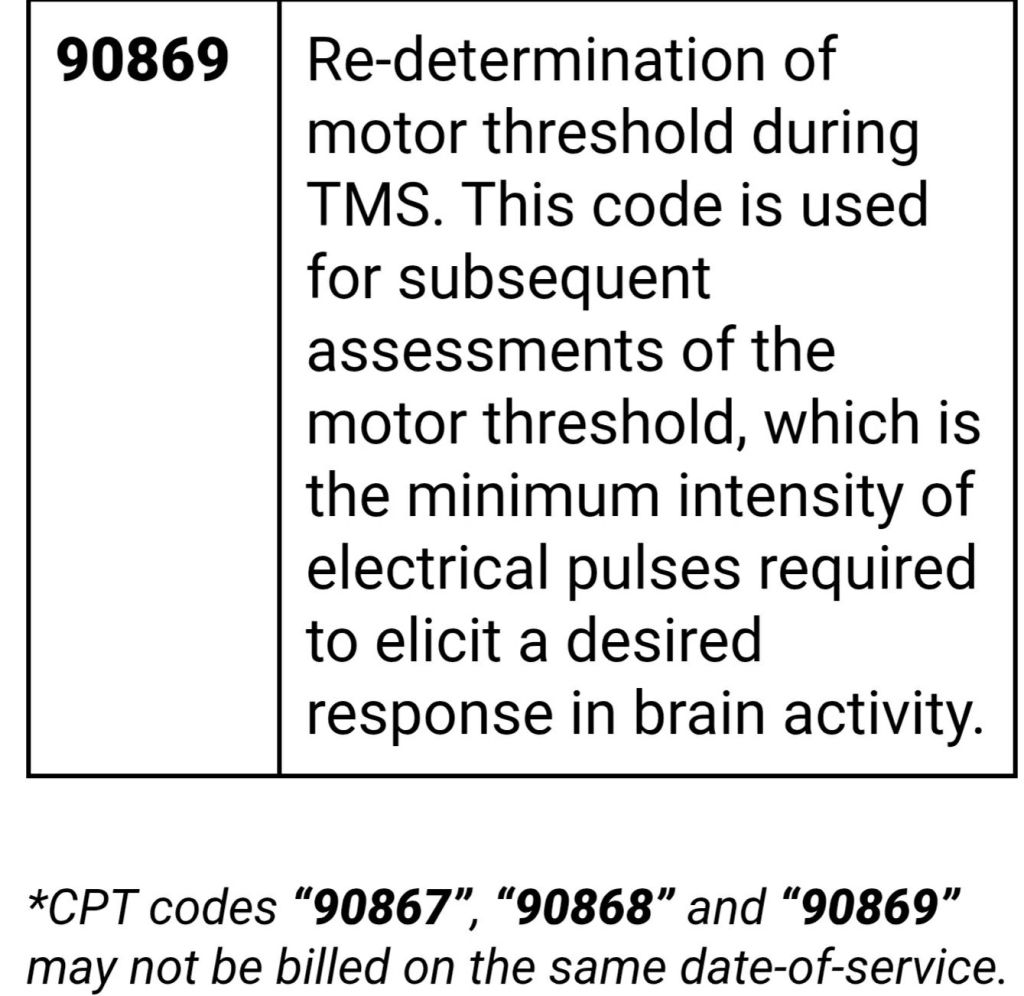
Coding: providers please use the following codes-
Criteria:
- Any patient 18 years and older
- With a DX of major depressive disorder (please see the image below)
- Documented failure to achieve a satisfactory clinical response following at least two trials of antidepressants at adequate dosage, duration, and adherence.
- TCM is not the first line treatment
Find this type of information useful? Follow my blog! Learn payer updates #medicalbilling #medicalcoding #reimbursement.
- UHC Community Health of Fl- new transportation provider
- Carolina Complete Health: radiology and diagnostic cardiology prior auth update
- NYS Medicaid: existing policy reminder coverage for SD/ED
- Carolina Complete Health: co-pays for pregnant members info
- HEDIS Measure: Lead Screening in Children (LSC)

Leave a comment