This policy applies to commercial plans for patients that are in the Neonatal Intensive Care Unit (NICU) and who were born at 32 weeks’ gestation or older, and where a genetic condition is suspected, are eligible for select rapid tests through a new genetics program.
Below are some important information regarding this new program.
What is the effective date for this program?
July 1,2021
Who is Eligible for this new program?
Patients that were born at 32 weeks gestation or above where a genetic condition is suspected by the provider are eligible for select rapid test. Please refer to the clinical indicator document for suggestions on when an underlying genetic condition may be suspected.
What genetic tests are included in the NICU Genetic Testing program?
Test options will continue to be evaluated and updated. At this time, rapid whole exome sequencing (rWES), available through XomeDxXpress® , analyzes the exome, which is the part of the genome that is thought to include most mutations that impact health.
Will the facility get reimbursed for the NICU Genetic Testing?
NO. The reimbursement will be only given to the participating laboratories directly.
How does this impact the facility’s current inpatient contract with UnitedHealthcare?
There is no impact to a facility’s current contract. The NICU Genetic Testing program is a new program, effective July 1, 2021, where tests pre-selected for inclusion in the program may be submitted directly to the approved laboratory for reimbursement. When a program approved test is utilized with the code UHC NICU, the laboratory will know to seek reimbursement from UnitedHealthcare directly and not the hospital.
Where to get more information?
• Laboratory Support: GeneDx has professionals, including genetic counselors, geneticists and clinicians, available to answer questions at no cost. For assistance, please contact GeneDx at Xpress@genedx.com, 888-729-1206.
• Genetic Counseling Services: InformedDNA, an in-network virtual genetic counseling practice, is available to provide pre-test and/or post-test genetic counseling and informed consent for genetic testing to the parents of your patients via telephone. To refer a patient, go to informeddna.com or call 800-975-4819. InformedDNA is in-network with most
UnitedHealthcare commercials plans.
What is RAPID (EXPEDITED) WHOLE EXOME SEQUENCING – TRIO (WES)?
Laboratory Proper Billing and coding:
81415 Exome (e.g., unexplained constitutional or heritable disorder or syndrome); sequence analysis
81416 Exome (e.g., unexplained constitutional or heritable disorder or syndrome); sequence analysis, each comparator exome (e.g., parents, siblings) (List separately in addition to code for primary procedure)
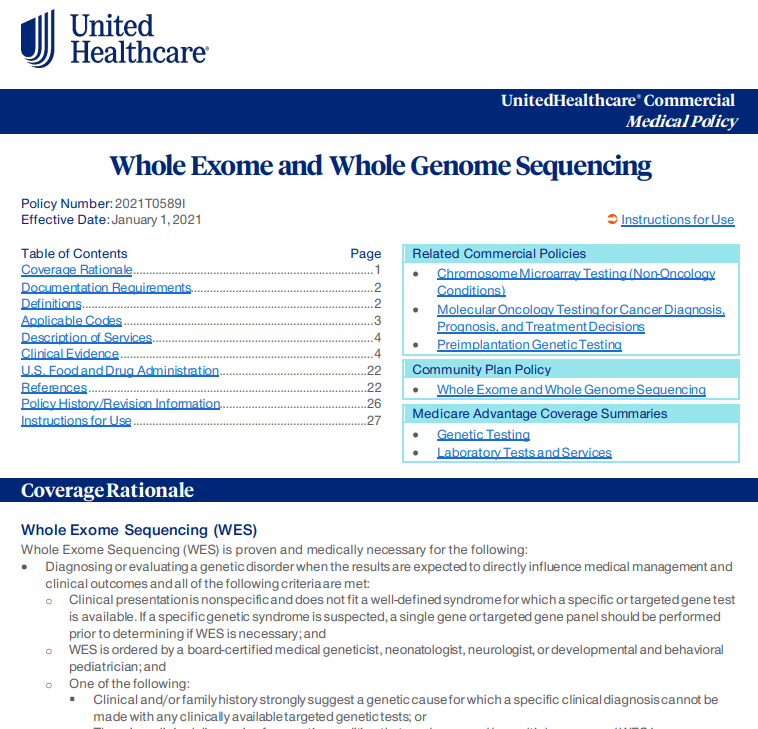
Partial Whole Exome and Whole Genome Sequencing medical policy:
Need to contact UHC ?
For more questions on NICU genetic testing, please contact United_Genetics@uhc.com.
To read the full Whole Exome and Whole Genome Sequencing, please click here.
- Aetna: reimbursement update ventral hernia
- UHC Medicare Advantage Plans: DME changes in certain States
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)