As of January 1, 2021 the following MVP Plans will no longer require prior authorization for High Tech Radiology Services:
MVP Medicare Advantage Plans
MVP Medicaid Managed Care
MVP Harmonious Health Plan (HARP)
MVP Child Health Plus (CHP)
These services include: MRI/MRA, PET Scan, Nuclear Cardiology, CT/CTA, and 3D Rendering Imaging Services
This applies only to the services rendered by IN Network Providers. For any of the above mentioned plans that do have Out of Network benefits and would like to go to an out of network provider: the Prior Authorization is Required!
To request an authorization: please complete a Prior Approval Request Form (PARF) and fax it to MVP at 1-800-280- 7346.
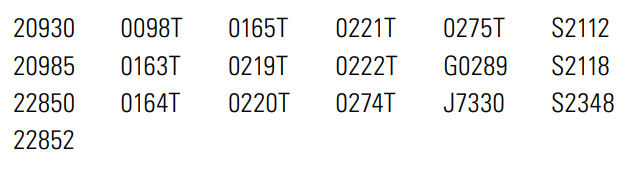
ALL other MVP plans still require a prior authorization for HIGH Radiology Services. To request an Auth please contact eviCore Healthcare by submitting requests at evicore.com or by calling 1-800-568-0458.
#MRI, #MRA, #PET, #MVPCHP, #MVPHARP