Effective 7/14/25 there is a new specialty pharmacy policy will apply to all of Emblem Health lines of busines: commercial, Medicare, medicaid.

This policy applies to all outpatient providers in the following place of service: outpatient hospital, physician office,home of the member and ambulatory infusion.
Takeaways:
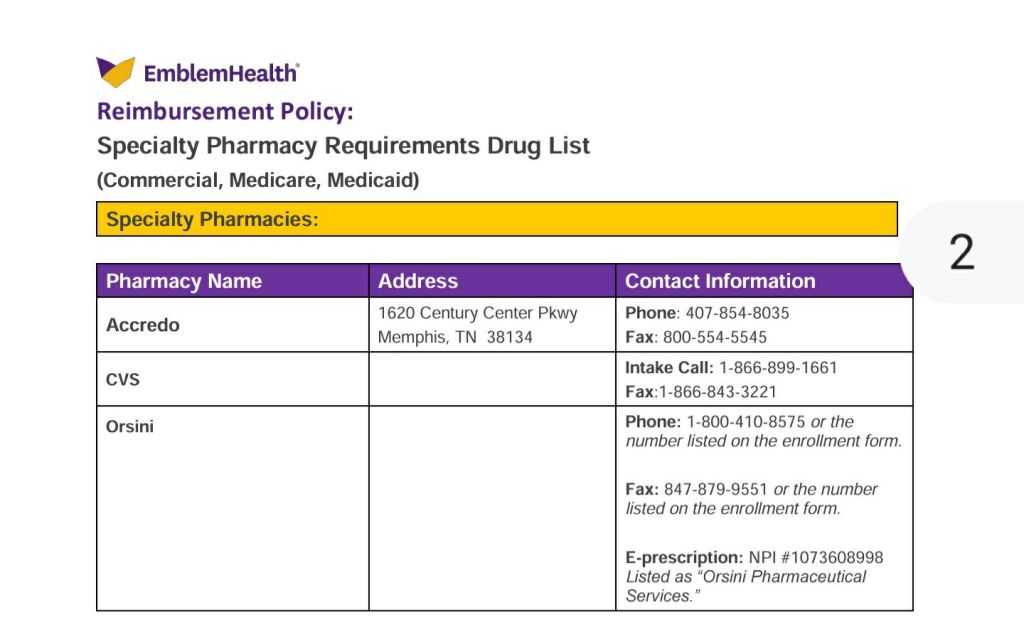
1. According to this policy the providers need to contact the respective specialty pharmacy to request prior auth and are only allowed to bill for specialty medications administration NOT the medication itself.
2. The Specialty Pharmacy will be allowed to bill Emblem health under the member’s medical benefit and receive reimbursement.
3. For any Medicaid EmblemHealth plan- the medicatin codes must be on Medicaid Fee Schedule. If the code is not listed it will not be reimbursed.
Exclusion: this policy does not apply to home infusion providers.
For a full list of specialty medications please visit Emblem Health for more information and a PDF version of the policy
Find this type of blog post useful? Subscribe to my blog and keep current with payer updates, medical billing and coding guidelines.

