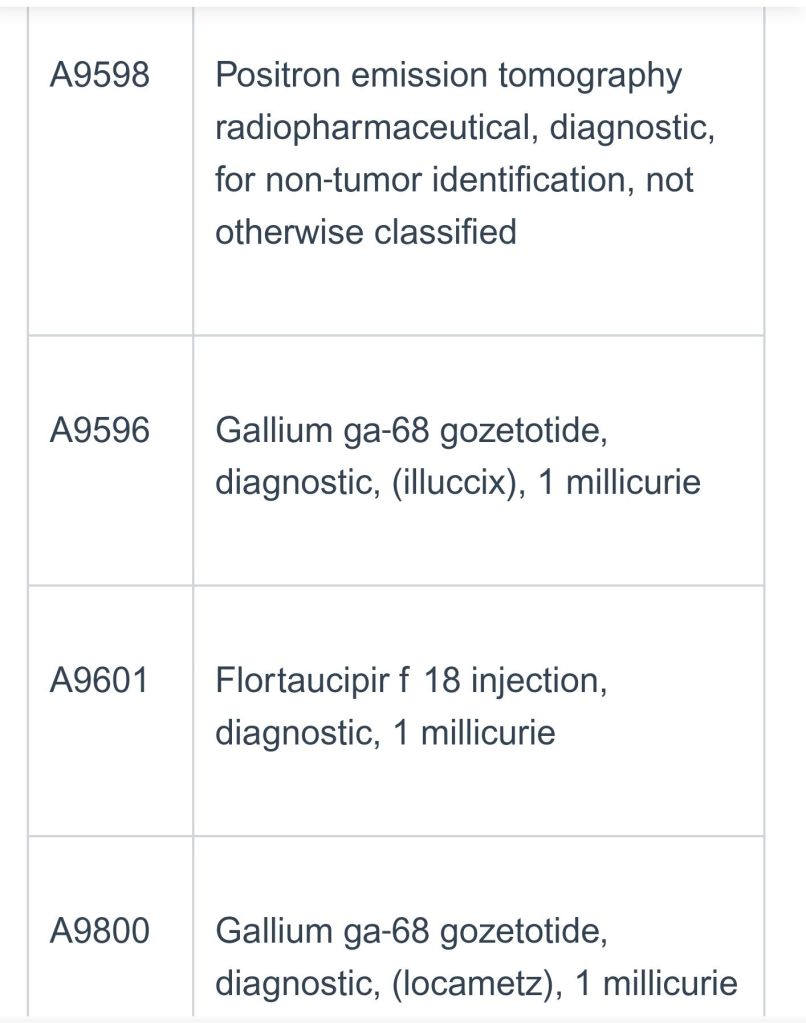
The following information will apply to any DOS on 12/1/25 and thereafter.
Starting 12/1/25 the PET tracer will require an auth in addition to PET services.
Please submit both PET and radiotracer codes- for prior authorization. The UM criteria for PET will not be affected. However both codes will be either approved or denied. Please note that the radiotracer must coorespond to the requested PET code.
The following codes will be affected:




Find this content useful? Follow my blog for more healthcare updates!