As the new year starts so do the change of theember ID changes and or group numbers.
Is your provider office aware of these changes?
Please note that for any 32BJ members there is a new TPA, group#, member ID, and cards.
Please note the new ID:
Effective Jan 1,2026- new members ID prefix BJVBJ.
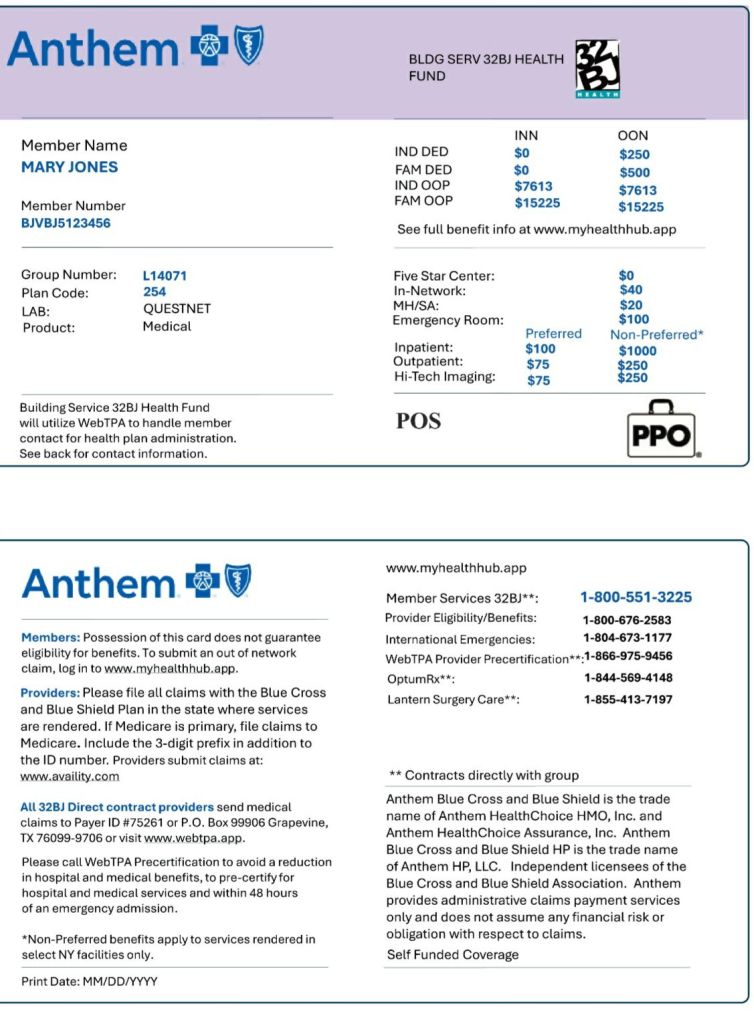
For OON probiders- please make sure to submit your claims directly to the TPA- WebTPA.
Find this type of information useful? Follow my blog!