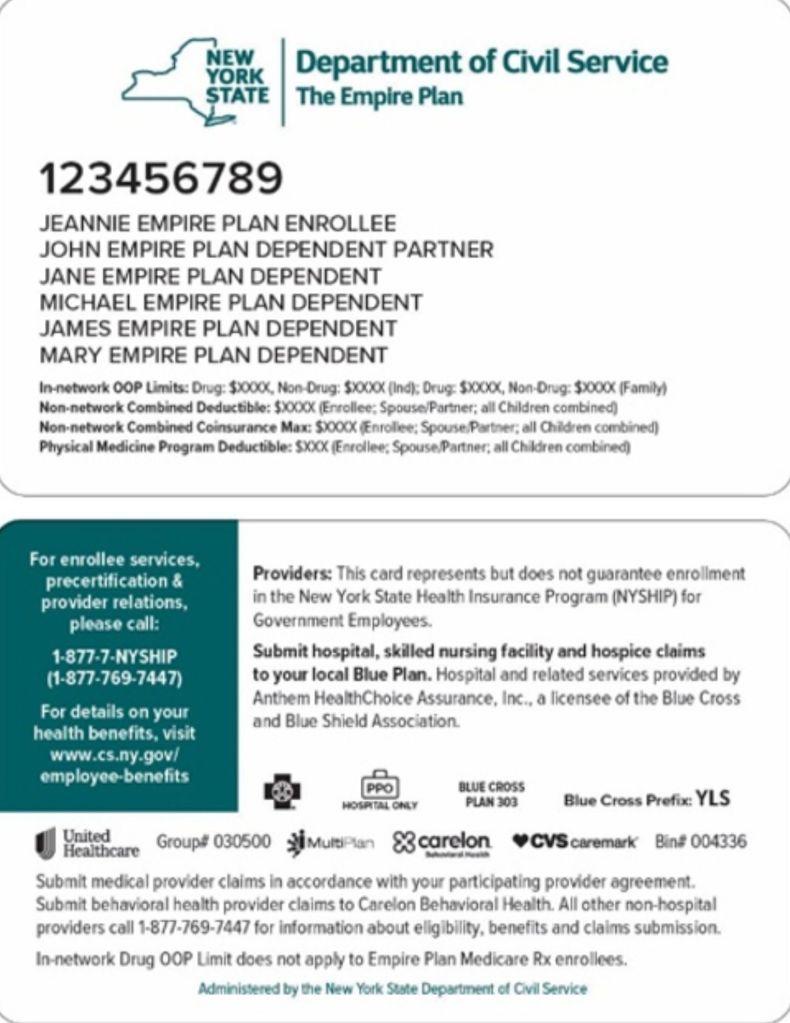
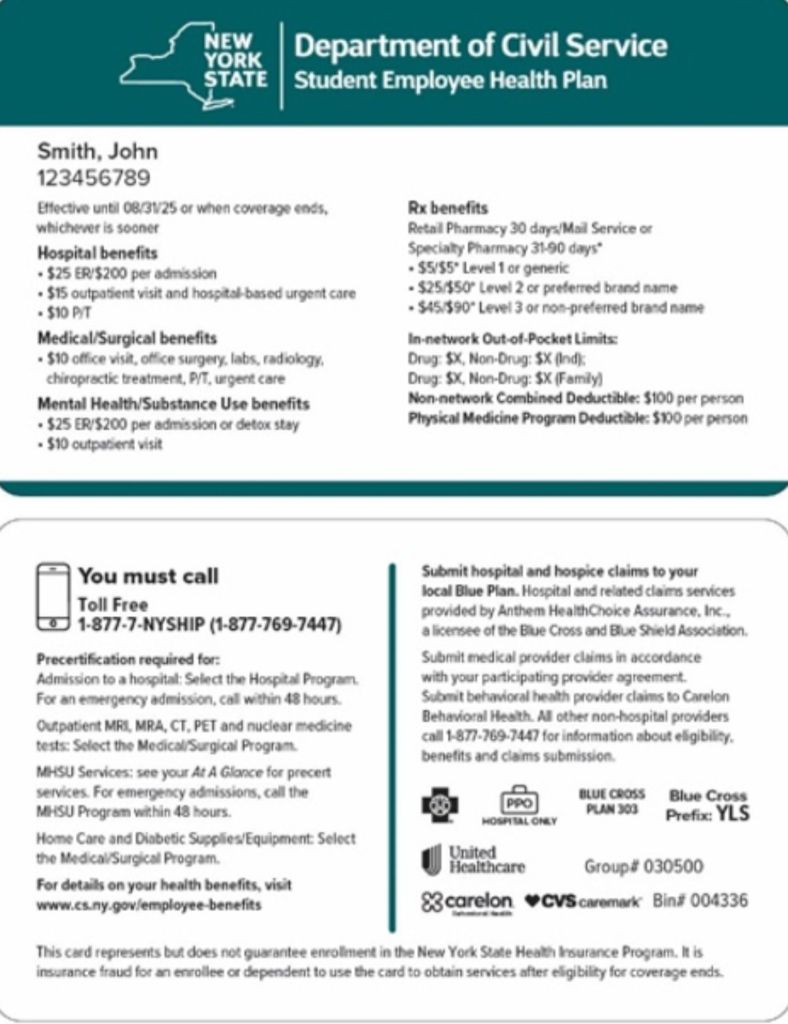
Please note that this address is only for official contract related notices and NOT for claims correspondence. For claims questions or submission/remittance please use the address that is on the back of the patient’s card.
You can also go on unitedhealthcare portal for reimbursement policies, fee schedules and/or contract and credentialing information. https://identity.onehealthcareid.com/oneapp/index.html#/login
New Mailing address:
UnitedHealthcare
Attn: Network Market VP MN103
6022 Blue Circle Drive
Minnetonka, MN 55343
Find this type of content useful? Follow my blog! #credentialling #contract #reimbursement #UHC