At the beginning of Covid 19 PHE and during, the insurance payers scrambled around to put together virtual care/telehealth/telemedicine policies. Since then, there were many revisions, so it is of no surprise when Cigna announced that they are adding some of the codes that were on non-permanent virtual list to their Virtual Care Reimbursement Policy.
These Codes are:
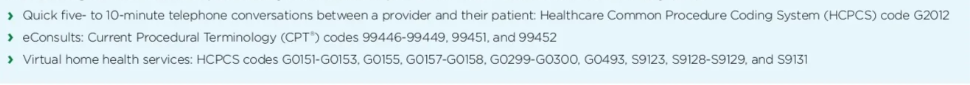
However, how can home health services like S9123–Nursing care, in the home; by registered nurse, per hour (use for general nursing care only, not to be used when CPT codes 99500-99602 can be used), code that is used for coding and billing Private Duty nursing Billing, be used as a virtual code? This code is used for MLTC members that require around the clock nursing care, members that cannot take care of themselves…so how are the services supposed to be done via “virtual care”?
Just my 2 cents….. 🙂
Would you like to read the full Cinga Virtual Care Reimbursement Policy? Click on this link: https://static.cigna.com/assets/chcp/secure/pdf/resourceLibrary/clinReimPolsModifiers/R31_Virtual_Care.pdf
Enjoy this type of content? Follow my blog for more up-to-date medical billing and coding information. #medicalbilling #medicalcoding #reimbursement #telehealth
Latest Blog Posts:
NYS Medicaid POC Syphilis testing coverage
Effective for any DOS August 2025 and thereafter Point of Care testing for Syphilis is covered for all fee fo service Medicaid and Managed Medicaid Members. Where is this test covered (POS)? physician/nurse practitioner/licensed midwife private office setting What kind of POC is covered and reimbursed? Currently there is only one FDA approved test -Clinical…
NYS Medicaid OBGYN CPT II codes reporting requirement
If you are a provider in NY and accept Managed Medicaid or Fee-for-service Medicaid plan types, then this blog post post is for you! For any DOS (for deliveries on July 1, 2024) and thereafter, the OBGYN providers billing bundled/global OBGYN codes, are also required to bill the following CPT II reporting codes. Global OBGYN…
NYS Medicaid: Bariatric Surgery Medical Policy Update
Do you accept NYS Medicaid or Managed Medicaid Plan members? Then this blog post is for you! Non surgical treatment should be attempted: ex. diet and increased exercise. Bariatric Surgery Adult Patient: 18 years old and over Pediatric patients: 18 years and older – patients that are deemed physically, mentally, and emotionally mature by a…


