According to EmblemHealth-for self funded plans: Local 389 Health and Welfare fund- for the DOS 9/1/23 and thereafter have a new timely filling date for submitting claims. The new date is 90 days after the services were rendered.
This new time frame applies to In network and Out of Network providers.
Types of claims: professional, facility and other provider types
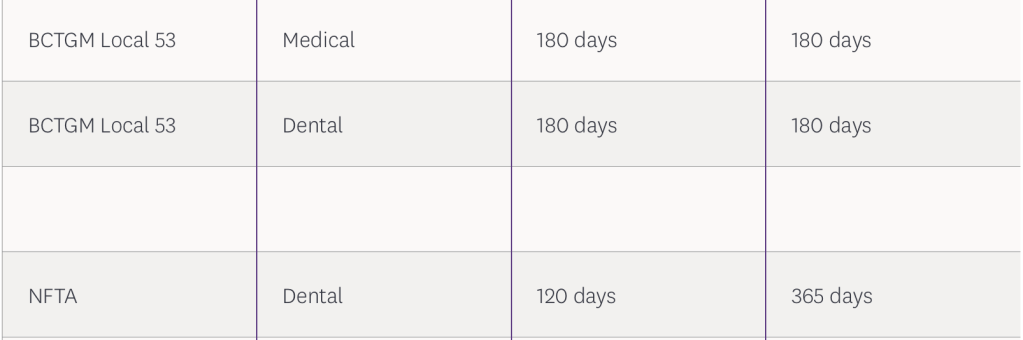
Please note that this change DOES NOT APPLY to the other ASOs (Administrative Service Organizations).
The following is still in affect:
Find this blog post useful? Then follow my blog for more medical billing and coding guideline updates and changes.
In a meantime check out my other blog posts:
Previous Blog Posts:
FidelisCare-concurrent prior auth update for family and group therapy services.
This update will apply to any dos of Jan 1, 2026 and thereafter. This update does not apply to SUD services/ providers that are certified as Article 32. 29-I providers are also excluded from the concurrent prior authorization requirenments. Services affected: Family Psychotherapy – CPT Code 90847 Group Psychotherapy – CPT Code 90853 FidelisCare members have 30…
Healthfirst Pharmacy Update Contrast agent reimbursement
The following information applies to the members in the following plans: Managed Medicaid Plans and Personal Wellness Plans (HARP) Back in 2023, NYS DOH announced that there will be a change to the pharmacy benefits for MMC, HARP members- the pharmacy benefits will be covered but NYRx. This change was finally implemented in April 2025.…
NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
The information discussed below applies to straight NYS Medicaid members for the DOS 10/1/25 and effective for any DOS on or 11/1/25 and thereafter for any Managed Medicaid Members. What is TC? A non-invasive form of brain stimulation using magnetic pulses on specific areas of the brain. This therapy is used to improve the symptoms…

