The Process will be in 2 phases.
Phase 1 will begin on 04/28/21- on or after this date BCBS NC will transition to Cover My Meds and the pharmacy call center team, from Care Radius.
Partial Lis of Phase 1 medications:

During Phase 1 providers should still use existing process (i.e., Care Radius or 800-571-7942), to request prior authorizations for medications that are NOT on the PHASE 1 list.
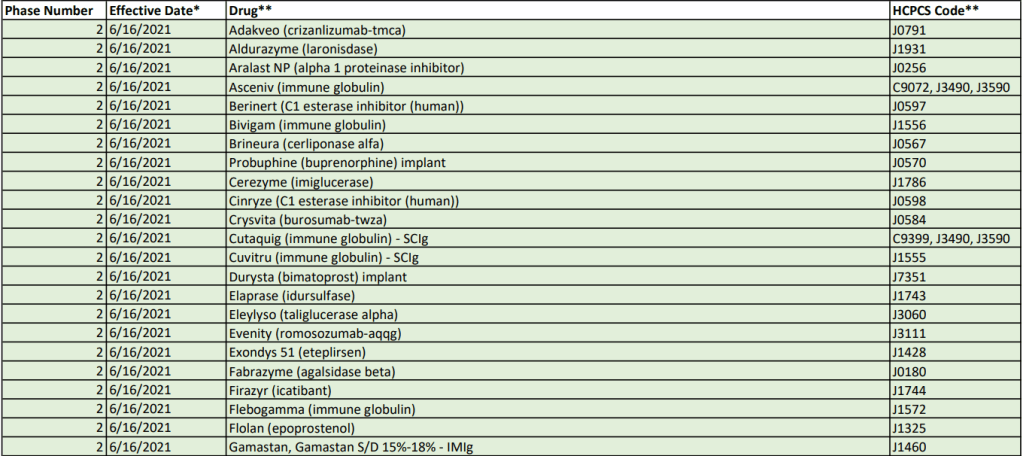
Phase 2- will begin on or after 06/16/2021 and providers will need to contact Cover My Meds or pharmacy call center team, to request an authorization.
Below is partial list for Phase 2 medications:
How to request an authorization:

Please note: Phase 1 medical drug Corporate Medical Policies and associated fax forms will be moving to www.bluecrossnc.com/umdrug. We will notify you when this shift occurs via another news article. Once this move occurs, you may notice some formatting/layout changes to policies. If there is a policy change, this will be communicated separately.
To see the whole list of Phase 1 and Phase 2 medications please click here.
#priorauthorizations, #medications, #covermymeds