Are you a a DME provider or a physician that prescribes DME for Emblem Health members? Then this blog post is for you!
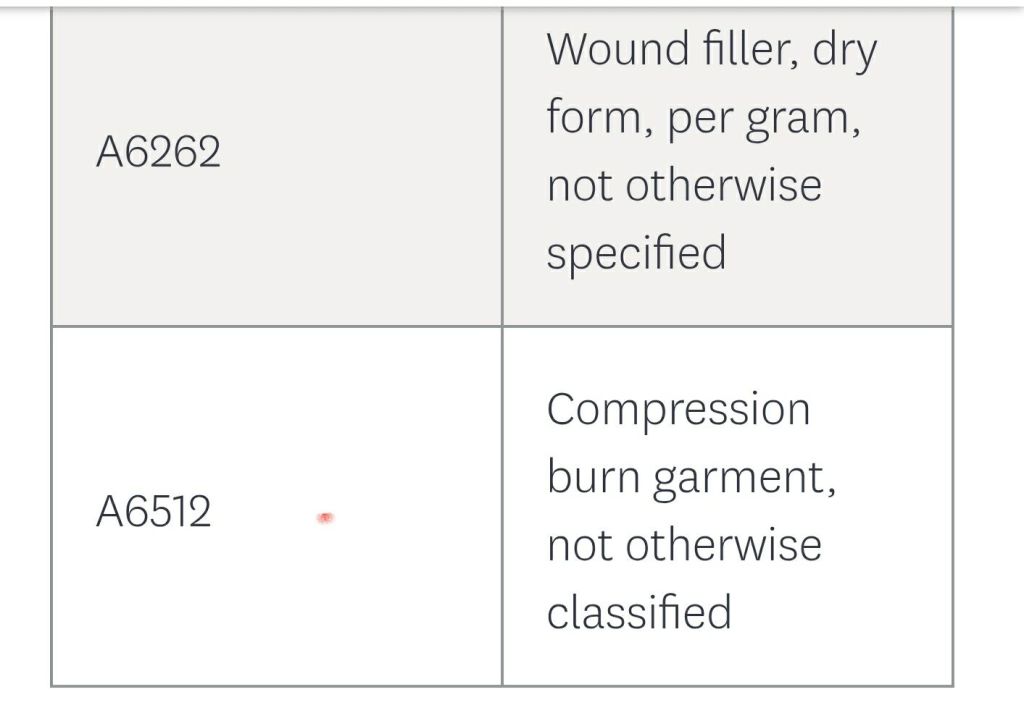
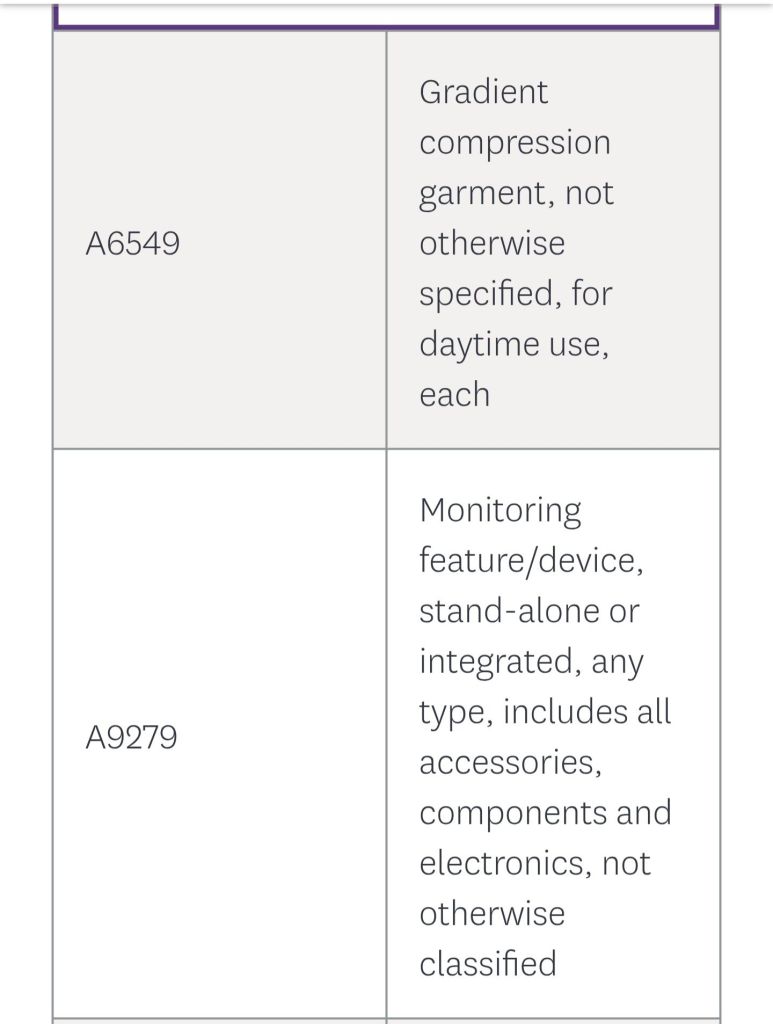
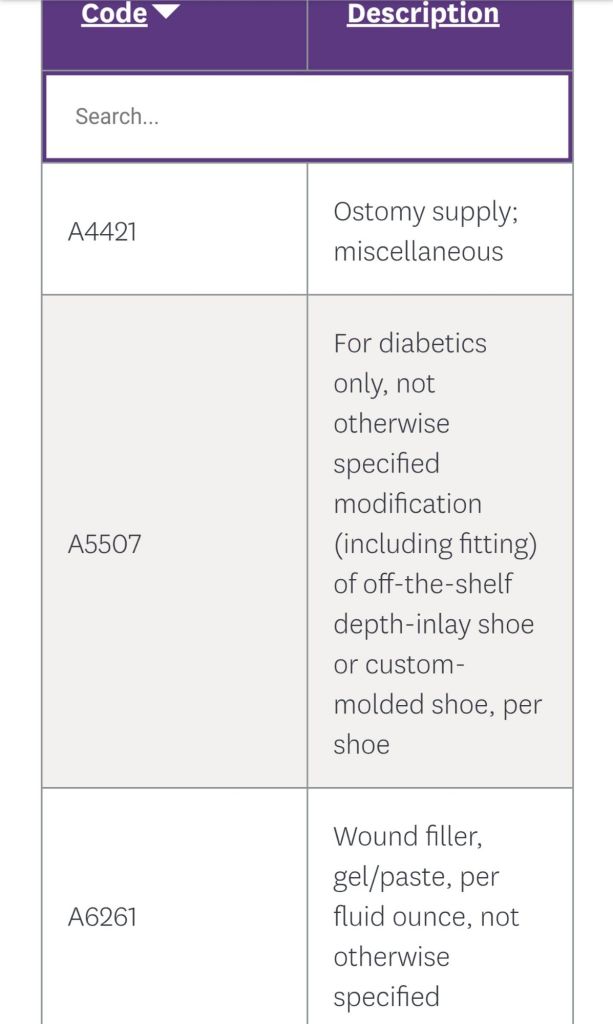
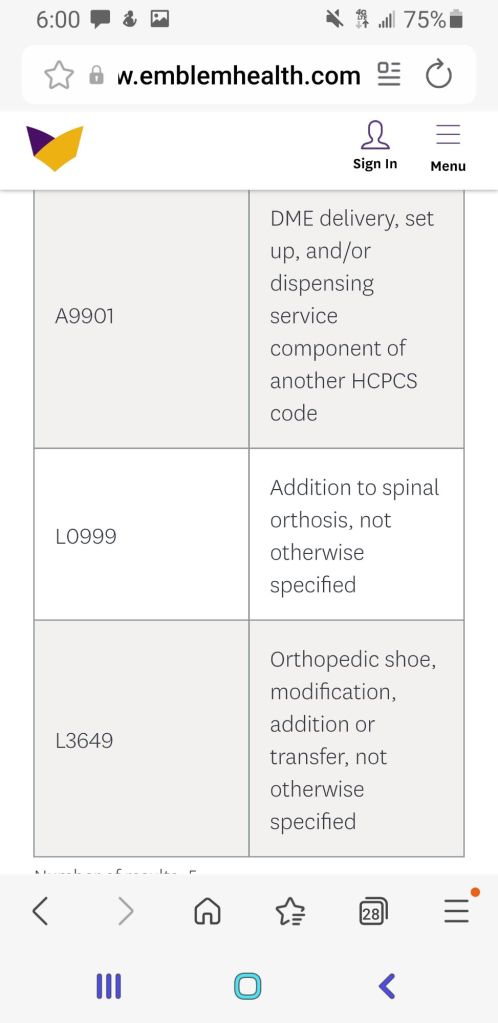
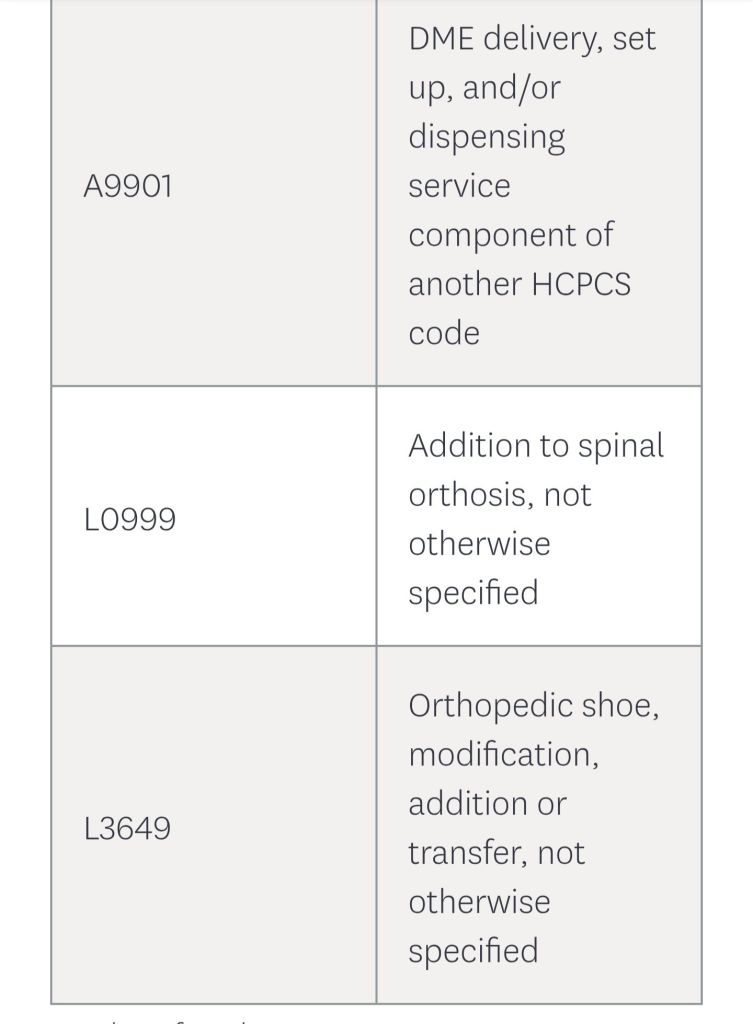
Starting on for any DOS 13,2026 and thereafter the following DME codes will be added to the prior authorization list.
If you find this type of content useful? Follow my blog for more!
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.