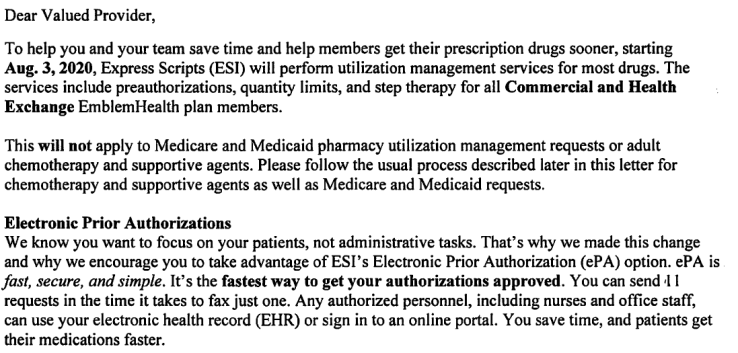
Just a reminder to all of providers that accept EmblemHealth Commercial and Exchange Plans- starting 08/03/2020 Express Scripts will be responsible for utilization management of most specialty and step therapy drugs (specialty medications).
This change does NOT apply to EmblemHealth Medicaid and Medicare Plans or adult chemotherapy and supportive agents. Providers should follow the prior authorization guidelines through EmblemHealth. (Please see below)
EmblemHealth Commercial and Exchange Plans– Requesting an EPA (electronic Prior Authorization) Steps:
1. If your practice utilizes an EHR, you would be able to order it electronically.
2. You may also utilize: Covermymeds, Surescipts or ExpressPath- here you are able to create a free account and request an ePA.
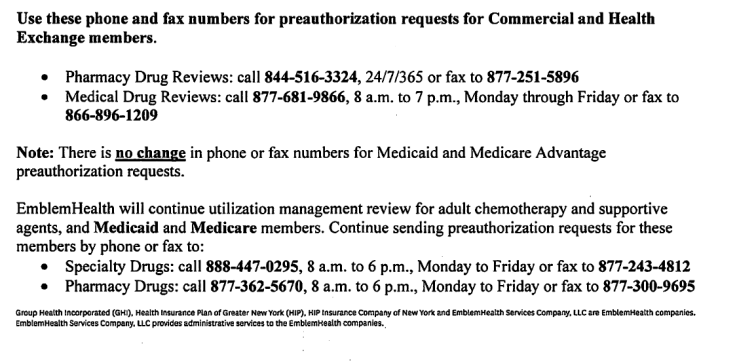
Request Prior Auth by Phone & Fax:
1. Pharmacy Drug Reviews- phone 844-516-3324 (available 24/7/365) or by fax#: 877-251-5896
2. Medical Drug Reviews- phone 877-681-9866 (available 8am to 7pm EST) Monday through Friday, or by fax#: 866-896-1209
***************************************************************************************
Requesting Prior Authorizations for EmblemHealth Medicaid and Medicare Plans:
1. Specialty Drugs- phone 888-447-0295 (available 8am to 6pm, Monday through Friday), or fax# 877-243-4812
2. Pharmacy Drugs- phone 877-362-5670 (available 8am to 6pm, Monday through Friday) or fax# 877-300-9695
IMPORTANT: if your patient has received an Authorization Approval prior to 08/03/2020, from EmblemHealth- it is valid until the expiration date of the authorization. Subsequent requests have to go through Express Scripts NOT EmblemHealth. (Your claims will be denied if you do not request an authorization from Express Scripts after 08/03/2020 and beyond)
For the full provider announcement, please see the slideshow below.