As of 01/01/2021-there are two main changes that will take effect:
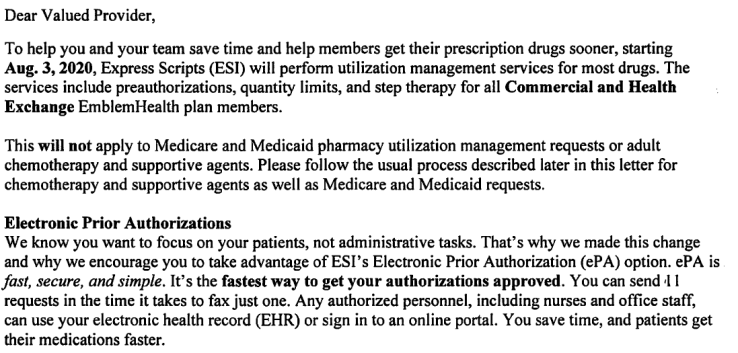
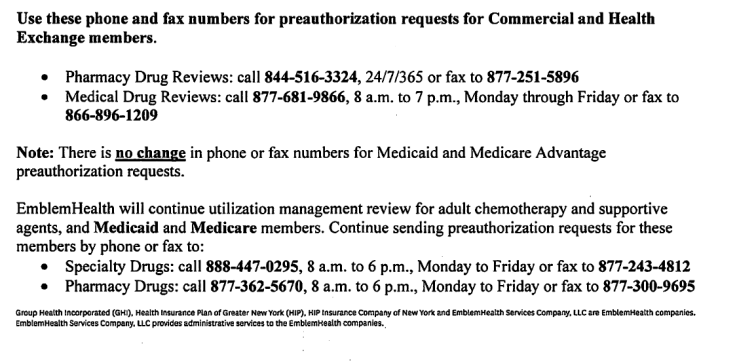
- Express Scripts will take over utilization management for drugs (medication) – this will apply to ALL lines of business including Medicaid and Medicare plans. The utilization management will include: prior authorizations, quantity limits and step therapy.
- New Century Health (NCH) will authorize most oncology related chemotherapy drugs and supportive agents, when these services are performed (delivered) in physician’s office, outpatient hospital, or ambulatory setting.
Note: #2 Change DOES NOT APPLY to Montefiore CMO, EmblemHealth Inc. (formerly GHI), members managed by HealthCareParners, or members under 18 years of age.
For complete list of drug formulary: Medicare Plans, click here
Note: Updates to the Commercial formulary apply to EmblemHealth, GHI, HIP and Vytra benefit plans. Updates to the Medicare formulary apply to EmblemHealth and ConnectiCare benefit plans. Exceptions will be noted.
#EmblemHealth, #HealthCarePartners, #Expressscripts, #NCH