In order for us to understand the coding difference between the nursing home visit codes and PDN (private duty nursing) codes, we need to go back to the basics.
Definitions:
Nursing Home services/visits- the necessary intermittent or part-time nursing care provided for a patient in the patient’s home or home substitute on a per visit basis. These services are usually no more than 2 hours per day and are performed by the Certified Home Health Agency.
Private Duty Nursing services/visits- nursing services that are one on one more personal level, for medical fragile members, that are performed on continuous basis. The purpose of Private Duty Nursing is to assist the caregiver/family members to help the member to remain safely at home. There is a separate code set for PDN services and a corresponding fee schedule.
Reimbursement:
Nursing Home Visits: are reimbursed in the increments of 15 min
PDN services/visits: are reimbursed by hour.
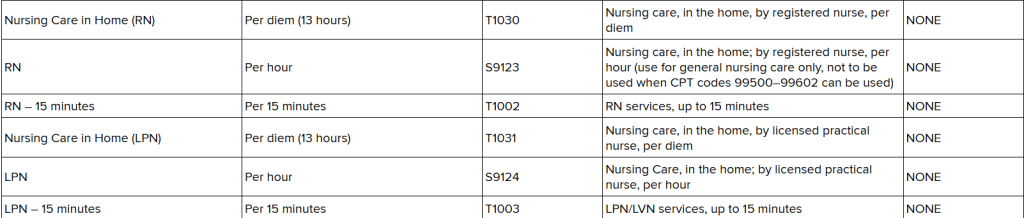
Exception: the following 2 code are reimbursed per diem because they represent the 13-hour shift
T1030- nursing care by RN, per diem, at home- 13 hour shirt
T1031- nursing care by LPN, per diem, at home- 13-hour shift
Coding–
I. Nursing Home Visits/Services:
a. T1002- RN services, up to 15 min
b. T1003- LPN services, up to 15 min
II. PDN services/visits:
a. S9123- RN services, per hour
b. S9124- LPN services, per hour
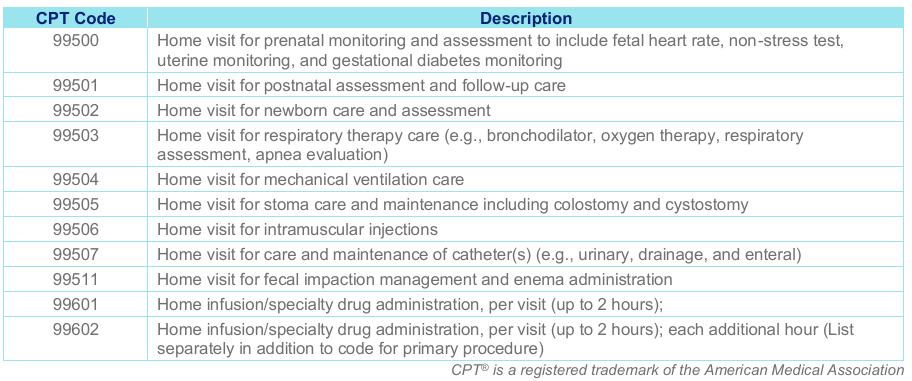
Please note that when you are billing the T codes you cannot bill them with the “other nursing codes” , listed below, or when the codes listed below better represent the nursing services that are authorized, performed.
Other Nursing Codes:
Need more information about NYS Medicaid Home and Community LTC codes: please visit here
PDN services fee schedule, here.
Find this type of content useful? Follow my blog for more payer updates, medical billing, coding updates, reimbursement updates!