For any DOS April 1st 2026 and thereafter the new company that will manage DME ordering and fulfillment will be Synergy Health.
This change will apply to Medicare Advantage Plans in certain states:
Individual HMO and PPO plans:
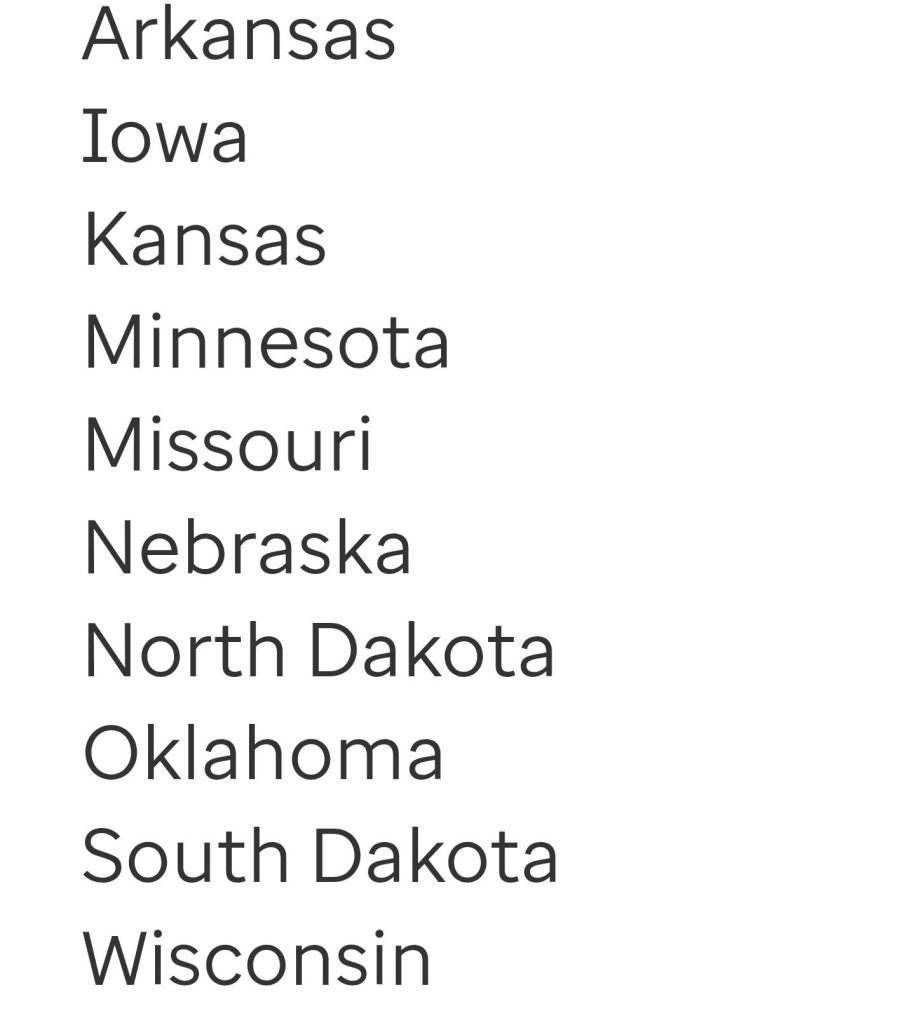
Chronic Special Needs Plans (C-SNP)

Dual Special Needs Plans (D-SNP):
- North Dakota
- South Dakota
- West Virginia
DME providers would need to join Synapse Health network. Synapse will contact you, however you can also reach out to them via email: JoinOurNetwork@synapsehealth.com
To which DMEs does this change apply?
- Diabetic supplies
- Enteral
- Home ambulatory
- Hospital beds
- Insulin therapy
- Mobility aids
- Negative pressure wound therapy
- Ostomy
- Oxygen
- Respiratory
- Respiratory vest
- Sleep
- Urological
- Ventilators
- Wheelchairs
The DMEs that this change does not apply to?
- Bone growth stimulators
- Cancer treatment
- Cardiac defibrillators
- Complex rehab
- Optune device
- Oral devices
- Orthotics
- Parenteral nutrition, vision, and hearing
- Prosthetics
Authorizations:
Providers would need to request an auth from Synapse Health for DOS of April 1st 2026 and there after, via their portal https://connect.synapsehealth.com/authorization/login
As a provider you can also go on their web to request a personalized training http://www.synapsehealth.com/welcome
Which plans are no affected by this change? Medicare Advantage-
Institutional Special Needs Plans (I-SNP)
Institutional Equivalent Special Needs Plans (IE-SNPs)
Group retiree plans
Find this type of content useful? Follow my blog for more payer updates: medical coding, billing, reimbursement, prior auth.

