The following information applies to the members in the following plans: Managed Medicaid Plans and Personal Wellness Plans (HARP)
Back in 2023, NYS DOH announced that there will be a change to the pharmacy benefits for MMC, HARP members- the pharmacy benefits will be covered but NYRx.
This change was finally implemented in April 2025.
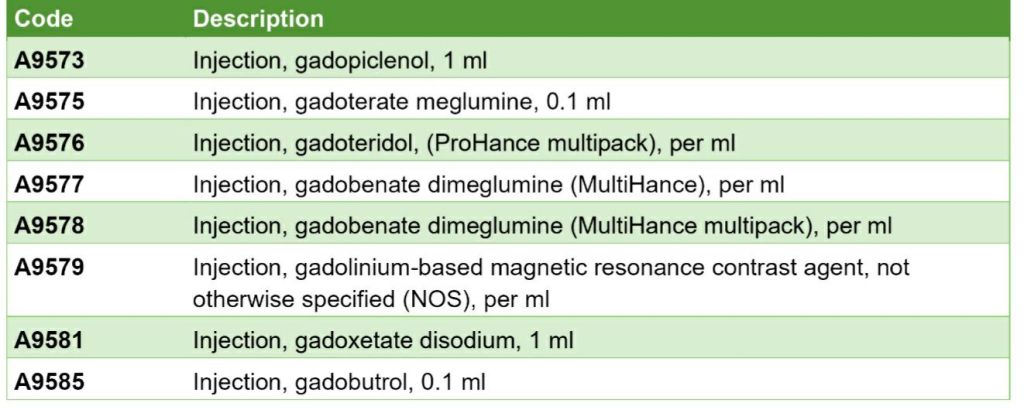
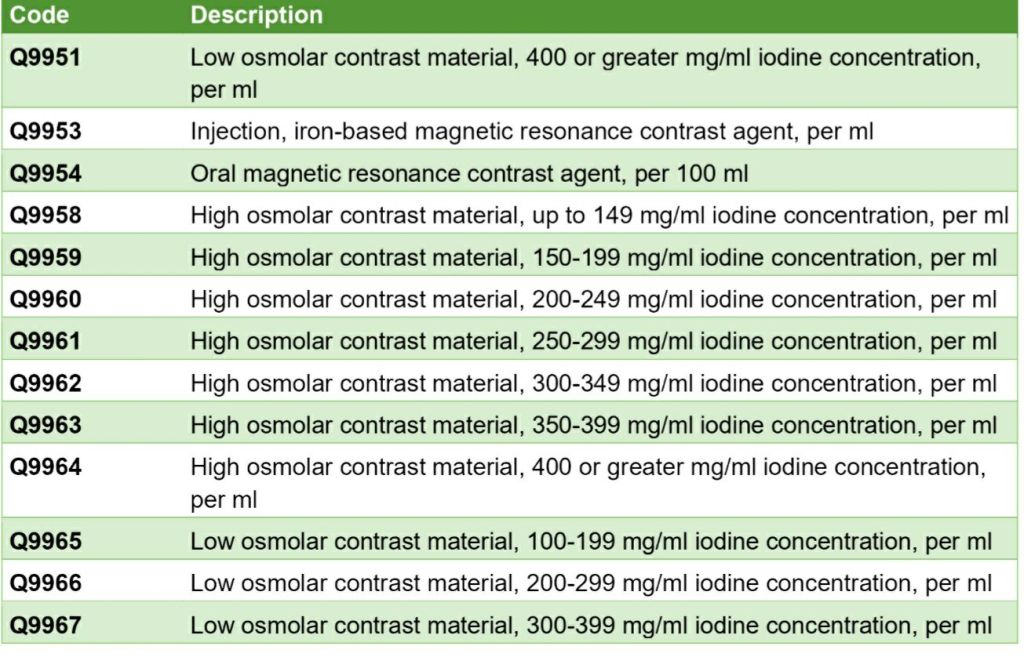
To align closer with this policy Healthfist will NO LONGER reimburse separately for the the following contrast agents used in radiological testing.
Coding: the following codes are affected:
NYS Medicaid Pharmacy website: information here
Find this information useful? Follow my blog for more payer updates #medicalbilling #medicalcoding #reimbursement #pharmacy
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.
- Aetna Medicare Advantage: reminder- certain post acute, skilled nursing and home health require pre- approval

