Starting Jan 1, 2026 certain nuclear imaging tests, OBGYN ultrasounds, and certain cardiology tests will no longer require a prior authorization for some of the following plan types:
1.UnitedHealthcare Insurance Company
2.UnitedHealthcare Mid-Atlantic, inc.
3.UnitedHealthcare Plan of the River Valley, Inc. and 4.UnitedHealthcare Insurance Company of the River Valley
5.Oxford Health Insurance, Inc.
United Healthcare Level Funded (formerly All Savers Life Insurance Company of California)
6.Neighborhood Health Partnership, Inc.
7.UnitedHealthcare Individual Exchange plans, also referred to as UnitedHealthcare Individual and Family ACA Marketplace plans
8.UnitedHealthcare Services, Inc.
9.UnitedHealthcare Community Plans
Some of the affected codes are:


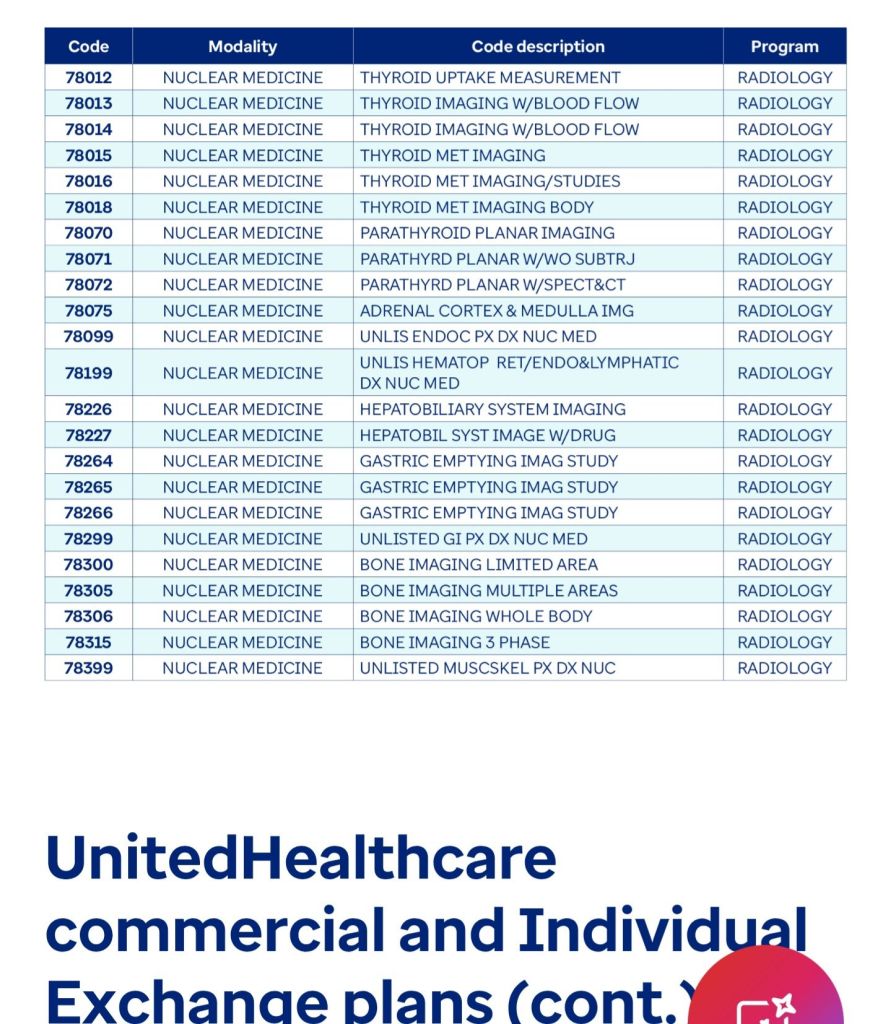
For a full list of affected codes please click here: https://www.uhcprovider.com/en/resource-library/news/2025/removal-prior-auth-radiology-cardiology.html
Find this content useful? Follow my Blog!
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.

