Are you a provider offering services to UHC Community Health dual eligible special need members? Then this blog post is for you!
As per recently passed bill: Texas House Bill 1open_in_new (Art. II, HHSC, Rider 32); there are new medical billing workflow that is in affect for any DOS 9/1/2025 and thereafter.
The following services will no longer be covered by Texas Health and Human Services Commission (HHSC).
Instead the providers would need to bill for any Medicare wrap around service to UnitedHealthcare Community Plan of Texas directly.
For any wrap around covered medications, including OTC- OptumRx will manage those.
Medicaid-covered services will switch from FFS to managed care billing based on the HHSC rate
Services provided through FFS for Medicaid-only beneficiaries, like pediatric nursing facility services, will not be affected
Some services and service would need a prior authorization.
For this the provider would need to go to UHCprovider.com and select Sign In at the top-right corner
- Sign in to the portal using your One Healthcare ID and password
- In the menu, select Prior Authorizations
- In the Prior Authorization and Notification tool, scroll down to “Create a new notification or prior authorization request” and click Create New Submissions
- Enter the required information and submit
If you need to find the list of the procedures and codes that require an auth please click here:
Listopen_in_new window- PDF
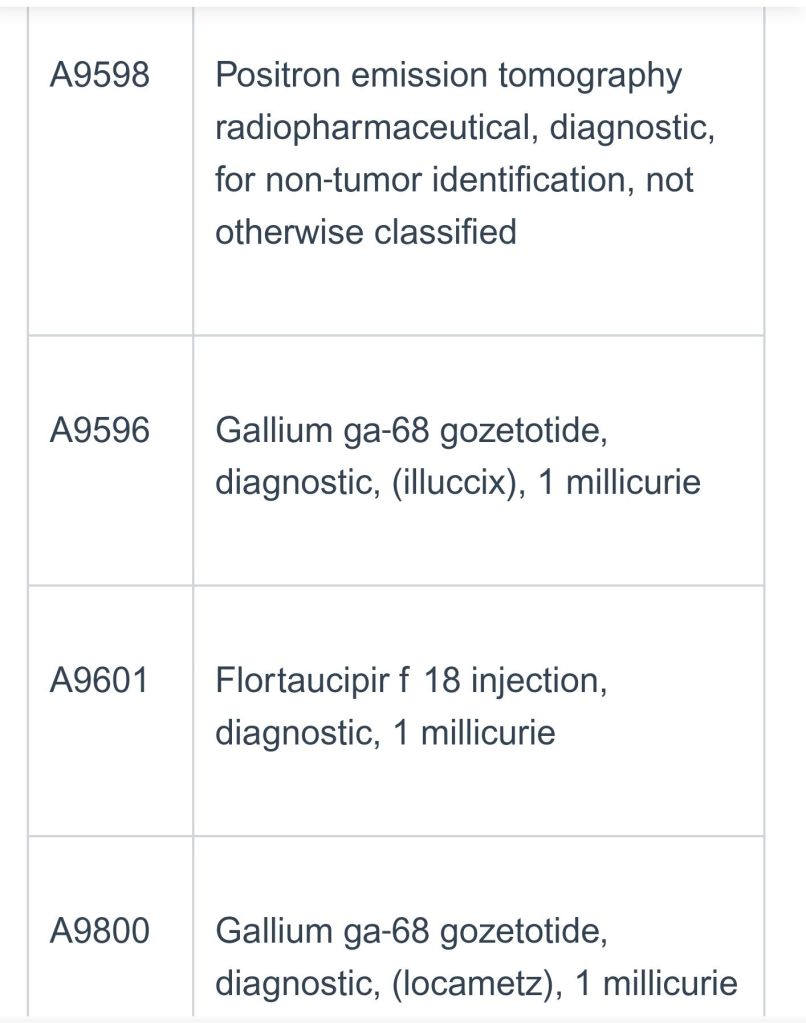
View all of the Rider 32 0rocedure codes and descriptions here: listingopen_in_new window
If you find this type of content useful? Please subscribe to my blog. I write about payer updates #medicalbilling #medicalcoding #reimbursement