For some specific DME equipment, prior auth requirenments will align with durable medical equipment (DME) prior authorization requirements of the UnitedHealthcare® Dual Complete® Special Needs Plan (DSNP).
These requirenments take effect on 10/1/25 and apply to members with UnitedHealthcare Community Plan District of Columbia as well as integrated DSNP plans for Long-Term Care Services and Supports (LTSS).
Some of these DMEs are:
Patient lifts
Power wheelchairs
Respiratory support devices
Among others.
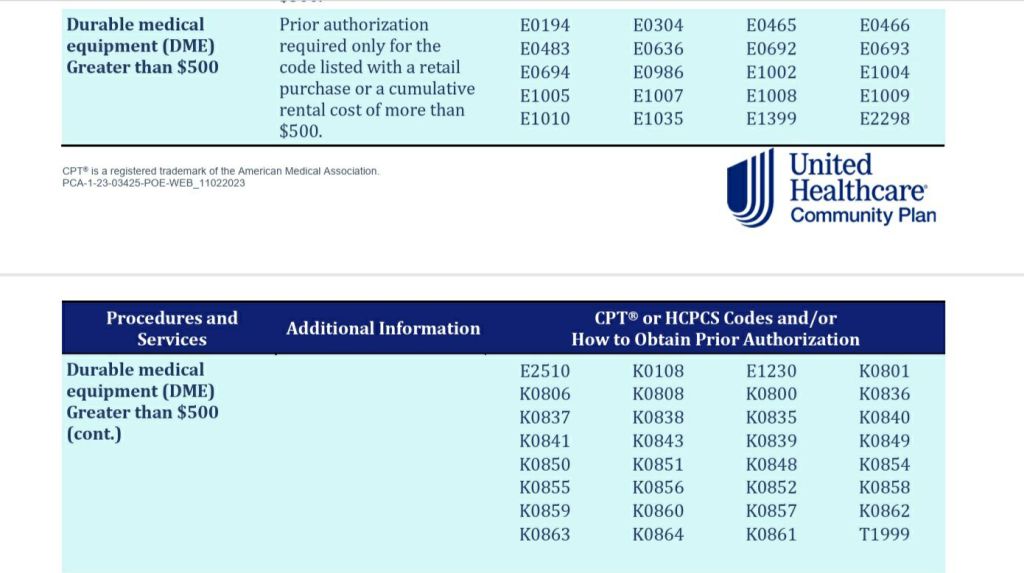
These prior authorization requirenments apply to the following codes:

To request an auth:
Phone: Call 888-702-2202
Fax: 866-968-7582. The fax form is available at Prior Authorization Forms on UHC website.
Or request the auth on the portal:
Sign in to the UnitedHealthcare Provider Portalopen_in_new with your One Healthcare ID
If you don’t have a One Healthcare ID, register now
From the left-hand tabs, select Prior Authorizations & Notifications
Was this blog post helpful? Then follow me for more payer updates!
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.

