HEDIS Measures get updated every year. In this post we will discuss the proper coding and billing for HEDIS Measure: Use of Imaging Studies for Lower Back Pain; and list the changes for the upcoming 2022 year. This measure applies to all types of insurances: Medicare, Commercial, and Medicaid.
Background:
One out of every four patients you see in your office has low back pain. The Centers for Disease Control and Prevention (CDC) reports that in the last three months, 25% of U.S. adults report having low back pain, making it second only to the common cold as a cause for lost work time and a primary reason for a doctor’s visit. Back pain will usually go away on its own. About 90 percent of patients with low back pain recover within six weeks.
What causes back pain?
HEDIS Measure: Use of Imaging Studies for Low Back Pain Definition-
Members 18-50 years of age with a new primary diagnosis of low back pain in an outpatient or ED visit who did not have an x-ray, CT or MRI within 28 days of the primary diagnosis. A higher score indicates appropriate treatment of low back pain (i.e., the proportion for whom imaging studies did not occur)
Proper Medical Coding:
CPT codes for imaging Studies-
List of Proper DX codes:
Measure Exclusions:
Exclusions include cancer, recent trauma, IV drug abuse, neurologic impairment, HIV, spinal infection, major organ transplant and prolonged use of corticosteroids.
Proper Exclusions Coding:
Improve the score for this HEDIS Measure:
-Avoid ordering diagnostic studies within 30 days of a diagnosis of new-onset back pain in the absence of red flags (e.g., cancer, recent trauma, neurologic impairment,
or IV drug abuse).
• Provide patient education on comfort measures, e.g., pain relief, stretching exercises, and activity level.
• Use correct exclusion codes if applicable (e.g., cancer).
• Look for other reason for visits for low back pain (e.g., depression, anxiety, narcotic dependency, psychosocial stressors, etc.).
• Document and code/bill all comorbidities (e.g. MVA, fall, trauma, etc.
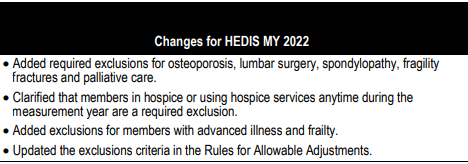
HEDIS Measure: Use of Imaging Studies for Low Back Pain 2022 Changes:
Find this content helpful? Follow my blog for more free medical billing and coding training.
Looking for a specific training? Coming soon the on-demand training/webinars. These webinars include a 10 question quiz and a 60 minute presentation. To read more about these webinars, please visit my on-demand training page. Pre-register today!
Recent Blog Posts: