Well-child visits in the first 30 months of life (W30):
Description: The percentage of members who had the following number of well-child visits with a PCP during the last 15 months. The following rates are reported:
- Well-child visits in the first 15 months. Children who turned 15 months old during the measurement year: six or more well-child visits.
- Well-child visits for age 15 month to 30 months. Children who turned 30 months old during the measurement year: two or more well-child visits.
Child and adolescent well-care visits:
Description: The percentage of members 3 to 21 years of age who had at least one comprehensive well-care visit with a PCP or an OB/GYN practitioner during the measurement year.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
In order to complete these measures AAP developed a comprehensive schedule.
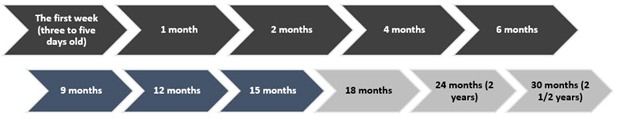
In order for Providers to comply with AAP, the providers should follow AAP recommendations: eight visits before their 30-month birthday (six visits before they are 15 months) with annual visits thereafter. The AAP periodicity schedule aligns with the well-child visits in the first 30 months of life (W30) HEDIS® measure. Ensuring all visits are completed before the child’s 30-month birthday is critical to assuring compliance with these measures.
For Empire BCBS NY Child Well Care visit coverage:
BCBS Empire NY offers complete coverage for well-child visits regardless of when visit is received:
Well-child visits (WCV) are covered 100% regardless of when the visit is received. Payment is not dependent on a set schedule, so there is no requirement to wait for a milestone birth month to schedule the well-child visit.

