This following policy is part of BCBS (NY) administrative policy guidelines (07/01/2021)
This blog post is for providers that need to meet the INR (in-home) monitoring quality measure.
What you will learn?
- What is INR monitoring Quality measure?
- Proper coding for in-home INR monitoring
- Documentation requirements to meet the INR in home monitoring measure
What is INR (International normalized ratio)?:
International normalized ratio (INR) is blood-clotting test. It is a test used to measure how quickly your blood forms a clot, compared with normal clotting time.
Background:
International normalized ratio is part of the 2021 Quality Measure Set (Pharmacy Quality Alliance (PQA) measures.
The QRS measure set is comprised of clinical quality measures, including the National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) measures and Pharmacy Quality Alliance (PQA) measures.
Previously, patients taking warfarin (brand name Coumadin) were heading off to the lab or clinic every few weeks for an international normalized ratio (INR) blood test. However, currently there is a small, portable device that patients on warfarin, can now self-test with a finger prick drop of blood.
Is there a provider type restriction for this quality Measure?
No, there is not provider type restriction.
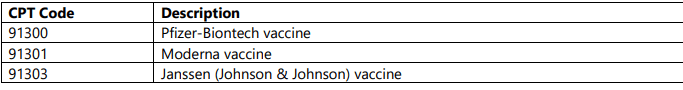
As a provider, which proper codes should I use for INR in-home patient monitoring?
Below please see the proper codes that providers should use for INR in-home patient monitoring.
Meeting INR monitoring Quality Measure:
Definition: The percentage of members 18 years of age and older who had at least one 56-day interval of warfarin therapy and who received at least one international normalized ratio (INR) monitoring test during each 56-day interval with active warfarin therapy.
Find this helpful? Follow my blog for more helpful blog posts about current medical billing/coding/reimbursement guidance.
If you are looking for more insightful breakdown of the medical coding and billing/reimbursement guidelines? Please check out my services page for more information.
Check out my latest Blog Posts below: