This policy applies to services performed in a facility: HCPCS and CPT codes
Aetna Better Health of Louisiana would like to remind providers that its Behavioral Health Reimbursement policy is aligned with the Louisiana Department of Health’s Medicaid Services. Providers need to check the Provider Manual regarding the proper billing practices for Behavioral Health Services. If the manual requires additional guidance for appropriate reimbursement, the details will be outlined by ABHLA in a supporting reimbursement policy.
To check the compliance with billing practices of the Louisiana Department of Health’s Medicaid Services, Aetna Better Health of Louisiana conducted an internal audit. ABHL found that many of the claims did not have the INDIVIDUAL PROVIDER as RENDERING provider but instead a FACILITY was listed as a rendering provider.
In order to comply with the proper billing and coding for these services, done in a facility setting, please put an INDIVIDUAL RENDERING PROVIDER NPI in the box 24J on the HCFA 1500.
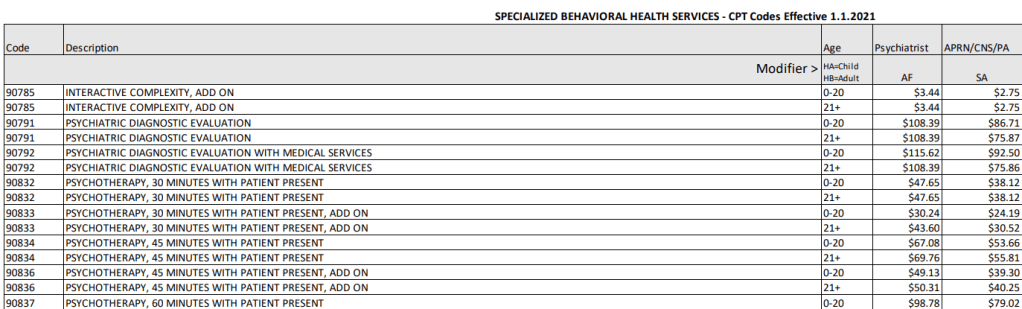
Below are just some codes that might have been paid previously (with a facility NPI):

Claims with the Facility NPI listed as the rendering provider will be denied and paid claims may
be recovered by the health plan. Should you receive denials for this reason, you may rebill your
denied claim(s) as a corrected claim with the Individual Provider NPI listed as rendering for
ABHLA to reprocess and pay the claim(s).
Please note that providers may see reimbursement impacted if not aligned to the Louisiana
Department of Health’s Medicaid services manual within 30 days of the date of this notification.
Below is just a partial list of the Louisiana Department of Health’s Medicaid Services: Behavioral Health Services Fee Schedule: