Below policy will apply to MVP plans that are located in New York and Vermont.
New York Virtual Care Cost-Share: Telemedicine
For MVP Medicare Advantage Plans- MVP will continue to apply the cost sharing waver for audio/visual and audio only until the DOS (dates of service) Dec 31,2021.
For MVP Commercial Plans- Starting August 1,2021 and thereafter the patients will have to pay their “in-person visit” cost-share for audio/visual and audio only visits according to their plan details.
Vermont Virtual Care Cost-Share: Telemedicine
For MVP Medicare Advantage Plans- MVP will continue to apply the cost sharing waver for audio/visual and audio only until the DOS (dates of service) Dec 31,2021.
For MVP Commercial Plans- Starting August 1,2021 and thereafter the patients will have to pay their “in-person visit” cost-share for audio/visual and audio only visits according to their plan details.
New York Covid-19 Treatment member Cost-Share:
Effective August 1, 2021, MVP will no longer waive the cost-share for COVID-19 treatment.
***Vermont Covid-19 Treatment member Cost-Share: ***
MVP will continue to cover COVID-19 treatment in full until March 1, 2022 as is required by
Vermont Rules.
COVID-19 Testing Member Cost-Share: NY &VT
MVP will continue to cover COVID-19 testing in full in New York and Vermont
COVID -19 Testing Coding and Billing Corner:
As of January 1, 2021 claims billed with a diagnosis code Z03.818 in conjunction with a COVID19 testing procedure code will be denied
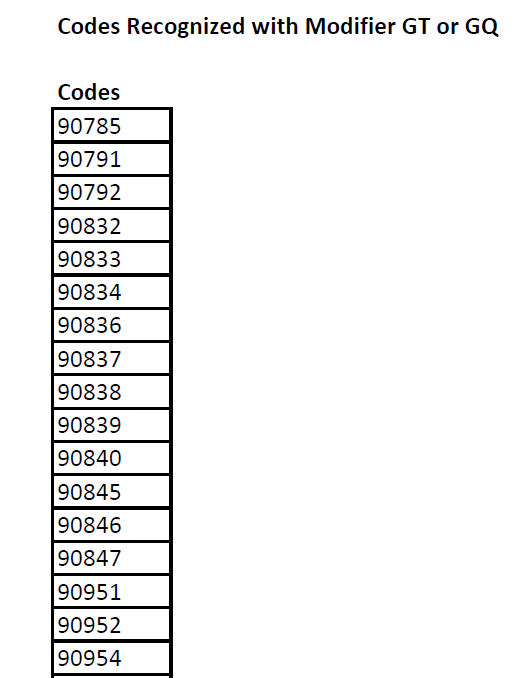
MVP will retain the expanded set of codes eligible for telehealth, consistent with CMS guidance, and will continue to monitor state and federal guidelines and regulations. In addition, MVP supports continued telehealth reimbursement and is currently reviewing coding guidance.
Find this information Helpful? Check out my other blog posts:
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.