HEDIS is always a hot topic of discussion. In this blog post we will discuss the HEDIS measure WCC or Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents.
Background/Research Data:
The research analyzed doctor visits pre-pandemic then during the pandemic period and the increases were dramatic. Overall obesity increased from 13.7% to 15.4%. Increases observed ranged from 1% in children aged 13 to 17 years to 2.6% for those aged 5 to 9 years.
The purpose of this HEDIS Measure:
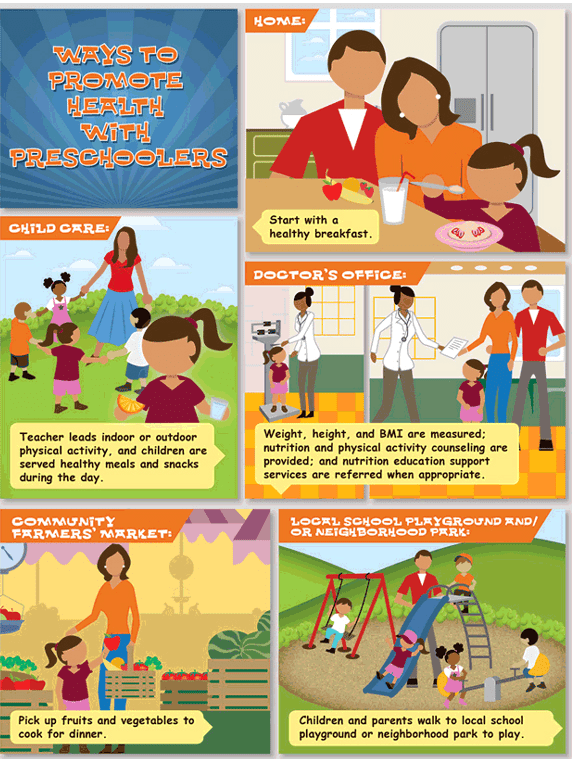
This HEDIS measure looks at the percentage of patients between the 3-17 years of age, who had an outpatient visit with a PCP or OB/GYN and have documented evidence for all the following during the measurement year:
- Body mass index (BMI) percentile (percentage, not value)
- Counseling for nutrition
- Counseling for physical activity
This HEDIS Measure (WCC) requires the following documentation:
- When counseling for nutrition, document current nutritional behavior, such as meal patterns, eating and diet habits, and weight counseling.
- When counseling for physical activity, document current physical activity behavior, such as exercise routine, participation in sports activities, bike riding and play groups.
- Handouts about nutrition and physical activity also count toward meeting this HEDIS measure when documented in the member’s health record.
Telehealth, virtual check-in, and telephone visits all meet the criteria for nutrition and physical activity counseling. Counseling does not need to take place only during a well-visit, WCC can also be completed during sick visits. Documenting guidance in your patient’s records is key.
Proper Coding and Billing:
Find this type of information helpful? Follow my blog for more free medical billing and medical coding training.
Recent Posts:
- FidelisCare-concurrent prior auth update for family and group therapy services.
- Healthfirst Pharmacy Update Contrast agent reimbursement
- NYS Medicaid to cover TCM (Therapeutic Transcranial Magnetic Stimulation)
- HealthFirst Telehealth mental health modifier update
- AETNA Commercial Plans: compression supplies non covered codes.